Indexed in: ESCI, Scopus, PubMed,
PubMed Central, CAS, DOAJ, KCI
PubMed Central, CAS, DOAJ, KCI
FREE article processing charge

Previous issues
- Page Path
- HOME > Browse Articles > Previous issues
Imagery
- "Reflection"
- J Yeungnam Med Sci. 2023;40(4):i. Published online March 17, 2023
- DOI: https://doi.org/10.12701/jyms.2023.00206

- 714 View
- 21 Download
Editorials
- Journal of Yeungnam Medical Science is indexed in Emerging Sources Citation Index (ESCI)
- So-Young Park
- J Yeungnam Med Sci. 2023;40(4):317-318. Published online October 12, 2023
- DOI: https://doi.org/10.12701/jyms.2023.01053

- 669 View
- 27 Download
- 1 Crossref
- Unveiling the challenges of diabetic foot infections: diagnosis, pathogenesis, treatment, and rehabilitation
- Chul Hyun Park
- J Yeungnam Med Sci. 2023;40(4):319-320. Published online October 11, 2023
- DOI: https://doi.org/10.12701/jyms.2023.01011

- 691 View
- 41 Download
Focused Review articles
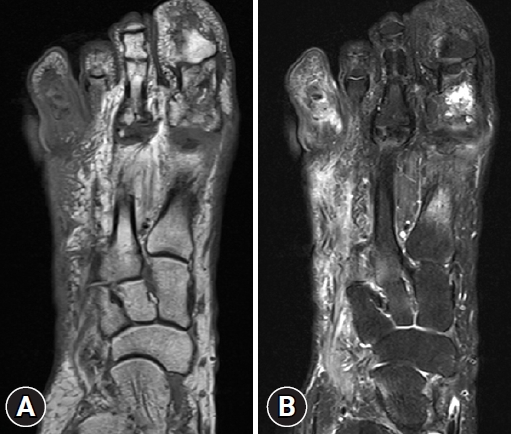
- State-of-the-art update for diagnosing diabetic foot osteomyelitis: a narrative review
- Inha Woo, Seung Jae Cho, Chul Hyun Park
- J Yeungnam Med Sci. 2023;40(4):321-327. Published online October 12, 2023
- DOI: https://doi.org/10.12701/jyms.2023.00976

- 1,206 View
- 73 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Recently, the International Working Group on the Diabetic Foot and the Infectious Diseases Society of America divided diabetic foot disease into diabetic foot infection (DFI) and diabetic foot osteomyelitis (DFO). DFI is usually diagnosed clinically, while numerous methods exist to diagnose DFO. In this narrative review, the authors aim to summarize the updated data on the diagnosis of DFO. An extensive literature search using “diabetic foot [MeSH]” and “osteomyelitis [MeSH]” or “diagnosis” was performed using PubMed and Google Scholar in July 2023. The possibility of DFO is based on inflammatory clinical signs, including the probe-to-bone (PTB) test. Elevated inflammatory biochemical markers, especially erythrocyte sedimentation rate, are beneficial. Distinguishing abnormal findings of plain radiographs is also a first-line approach. Moreover, sophisticated modalities, including magnetic resonance imaging and nuclear medicine imaging, are helpful if doubt remains after a first-line diagnosis. Transcutaneous bone biopsy, which does not pass through the wound, is necessary to avoid contaminating the sample. This review focuses on the current diagnostic techniques for DFOs with an emphasis on the updates. To obtain the correct therapeutic results, selecting a proper option is necessary. Based on these numerous diagnosis modalities and indications, the proper choice of diagnostic tool can have favorable treatment outcomes.
-
Citations
Citations to this article as recorded by- Unveiling the challenges of diabetic foot infections: diagnosis, pathogenesis, treatment, and rehabilitation
Chul Hyun Park
Journal of Yeungnam Medical Science.2023; 40(4): 319. CrossRef
- Unveiling the challenges of diabetic foot infections: diagnosis, pathogenesis, treatment, and rehabilitation
- The pathophysiology of diabetic foot: a narrative review
- Jiyoun Kim
- J Yeungnam Med Sci. 2023;40(4):328-334. Published online October 5, 2023
- DOI: https://doi.org/10.12701/jyms.2023.00731
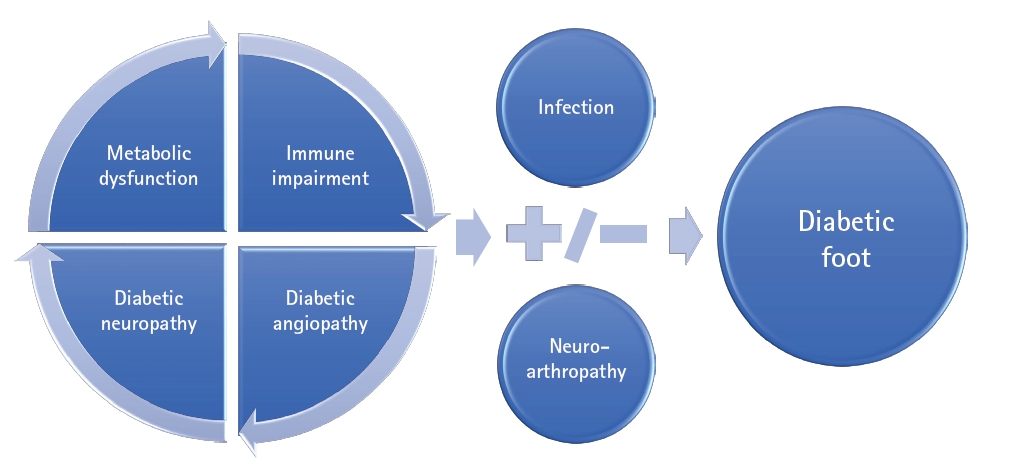
- 4,830 View
- 370 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - An aging population and changes in dietary habits have increased the incidence of diabetes, resulting in complications such as diabetic foot ulcers (DFUs). DFUs can lead to serious disabilities, substantial reductions in patient quality of life, and high financial costs for society. By understanding the etiology and pathophysiology of DFUs, their occurrence can be prevented and managed more effectively. The pathophysiology of DFUs involves metabolic dysfunction, diabetic immunopathy, diabetic neuropathy, and angiopathy. The processes by which hyperglycemia causes peripheral nerve damage are related to adenosine triphosphate deficiency, the polyol pathway, oxidative stress, protein kinase C activity, and proinflammatory processes. In the context of hyperglycemia, the suppression of endothelial nitric oxide production leads to microcirculation atherosclerosis, heightened inflammation, and abnormal intimal growth. Diabetic neuropathy involves sensory, motor, and autonomic neuropathies. The interaction between these neuropathies forms a callus that leads to subcutaneous hemorrhage and skin ulcers. Hyperglycemia causes peripheral vascular changes that result in endothelial cell dysfunction and decreased vasodilator secretion, leading to ischemia. The interplay among these four preceding pathophysiological factors fosters the development and progression of infections in individuals with diabetes. Charcot neuroarthropathy is a chronic and progressive degenerative arthropathy characterized by heightened blood flow, increased calcium dissolution, and repeated minor trauma to insensate joints. Directly and comprehensively addressing the pathogenesis of DFUs could pave the way for the development of innovative treatment approaches with the potential to avoid the most serious complications, including major amputations.
-
Citations
Citations to this article as recorded by- Diabetic foot – prevention and control challenges
Vitorino Modesto dos Santos, Taciana Arruda Modesto Sugai, Lister Arruda Modesto dos Santos
Belize Journal of Medicine.2024;[Epub] CrossRef - Integrated genetic analysis of diabetic complications: Bioinformatics insights into foot ulcers, neuropathy and peripheral artery disease
Jiaru Liang, Xiaoyang Gong, Xuyang Hu, Chong You, Jiaqi Zhou, Yuling Gao, Junwei Zong, Yong Liu
International Wound Journal.2024;[Epub] CrossRef - Unveiling the challenges of diabetic foot infections: diagnosis, pathogenesis, treatment, and rehabilitation
Chul Hyun Park
Journal of Yeungnam Medical Science.2023; 40(4): 319. CrossRef
- Diabetic foot – prevention and control challenges
- Management of diabetic foot ulcers: a narrative review
- Jahyung Kim, Otgonsaikhan Nomkhondorj, Chi Young An, Ye Chan Choi, Jaeho Cho
- J Yeungnam Med Sci. 2023;40(4):335-342. Published online September 22, 2023
- DOI: https://doi.org/10.12701/jyms.2023.00682

- 2,798 View
- 214 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Diabetic foot ulcers (DFUs) are among the most serious complications of diabetes and are a source of reduced quality of life and financial burden for the people involved. For effective DFU management, an evidence-based treatment strategy that considers the patient's clinical context and wound condition is required. This treatment strategy should include conventional practices (surgical debridement, antibiotics, vascular assessment, offloading, and amputation) coordinated by interdisciplinary DFU experts. In addition, several adjuvant therapies can be considered for nonhealing wounds. In this narrative review, we aim to highlight the current trends in DFU management and review the up-to-date guidelines.
-
Citations
Citations to this article as recorded by- Kick-Starting Wound Healing: A Review of Pro-Healing Drugs
Bethany L. Patenall, Kristyn A. Carter, Matthew R. Ramsey
International Journal of Molecular Sciences.2024; 25(2): 1304. CrossRef - Unveiling the challenges of diabetic foot infections: diagnosis, pathogenesis, treatment, and rehabilitation
Chul Hyun Park
Journal of Yeungnam Medical Science.2023; 40(4): 319. CrossRef
- Kick-Starting Wound Healing: A Review of Pro-Healing Drugs
- Management and rehabilitation of moderate-to-severe diabetic foot infection: a narrative review
- Chi Young An, Seung Lim Baek, Dong-Il Chun
- J Yeungnam Med Sci. 2023;40(4):343-351. Published online September 19, 2023
- DOI: https://doi.org/10.12701/jyms.2023.00717
- 1,836 View
- 116 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Diabetic foot is one of the most devastating consequences of diabetes, resulting in amputation and possibly death. Therefore, early detection and vigorous treatment of infections in patients with diabetic foot are critical. This review seeks to provide guidelines for the therapy and rehabilitation of patients with moderate-to-severe diabetic foot. If a diabetic foot infection is suspected, bacterial cultures should be initially obtained. Numerous imaging studies can be used to identify diabetic foot, and recent research has shown that white blood cell single-photon emission computed tomography/computed tomography has comparable diagnostic specificity and sensitivity to magnetic resonance imaging. Surgery is performed when a diabetic foot ulcer is deep and is accompanied by bone and soft tissue infections. Patients should be taught preoperative rehabilitation before undergoing stressful surgery. During surgical procedures, it is critical to remove all necrotic tissue and drain the inflammatory area. It is critical to treat wounds with suitable dressings after surgery. Wet dressings promote the formation of granulation tissues and new blood vessels. Walking should begin as soon as the patient’s general condition allows it, regardless of the wound status or prior walking capacity. Adequate treatment of comorbidities, including hypertension and dyslipidemia, and smoking cessation are necessary. Additionally, broad-spectrum antibiotics are required to treat diabetic foot infections.
-
Citations
Citations to this article as recorded by- Unveiling the challenges of diabetic foot infections: diagnosis, pathogenesis, treatment, and rehabilitation
Chul Hyun Park
Journal of Yeungnam Medical Science.2023; 40(4): 319. CrossRef
- Unveiling the challenges of diabetic foot infections: diagnosis, pathogenesis, treatment, and rehabilitation
Review article
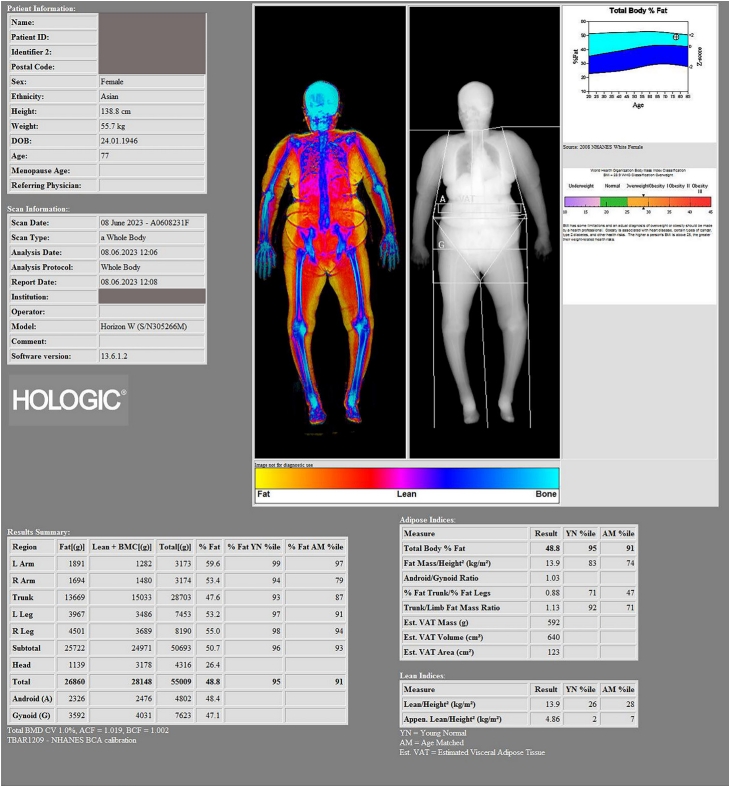
- Multidisciplinary approach to sarcopenia: a narrative review
- Wook Tae Park, Oog-Jin Shon, Gi Beom Kim
- J Yeungnam Med Sci. 2023;40(4):352-363. Published online September 7, 2023
- DOI: https://doi.org/10.12701/jyms.2023.00724
- 2,526 View
- 148 Download
-
 Abstract
Abstract
 PDF
PDF - Sarcopenia is a condition in which muscle mass and strength are decreased and muscle function is impaired. It is an indicator of frailty and loss of independence in older adults. It is also associated with increased physical disability, which increases the risk of falls. As a multifactorial disease, sarcopenia is caused by a combination of factors including aging, hormonal changes, nutritional deficiencies, and physical inactivity. Understanding the underlying pathophysiology of sarcopenia and identifying its different causes is critical to developing effective prevention and treatment strategies. This review summarizes the pathophysiology, consequences, diagnostic methods, and multidisciplinary approaches to sarcopenia.
Original articles
- Long-term supplementation with a combination of beta-hydroxy-beta-methylbutyrate, arginine, and glutamine for pressure ulcer in sedentary older adults: a retrospective matched case-control study
- Igor Kisil, Yuri Gimelfarb
- J Yeungnam Med Sci. 2023;40(4):364-372. Published online February 16, 2023
- DOI: https://doi.org/10.12701/jyms.2022.00899

- 2,182 View
- 139 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Growing evidence suggests that beta-hydroxy-beta-methylbutyrate (HMB), arginine (Arg), and glutamine (Gln) positively affect wound recovery. This study investigated the effects of long-term administration of HMB/Arg/Gln on pressure ulcer (PU) healing in sedentary older adults admitted to geriatric and rehabilitation care facilities.
Methods
This was a pilot retrospective case (standard of care and HMB/Arg/Gln)-control (standard of care alone) clinical study. Outcome measures were relative healing rates and Pressure Ulcer Scale for Healing (PUSH) scores (calculated after 4, 8, 12, 16, and 20 weeks) and time to healing.
Results
The study subpopulation was comprised of 14 participants (four males, 28.6%) with the median age of 85.5 years (interquartile range [IQR], 82.0–90.2 years). The control subpopulation was comprised of 31 participants (18 males, 58.1%) with the median age of 84.0 years (IQR, 78.0–90.0 years). At the beginning of follow-up, there were no statistically significant demographic (sex and age) and clinical (main diagnosis, baseline area, and PU perimeter) differences between the groups. During the study period, there were no significant differences in the relative healing rates and PUSH scores between the subpopulations. The median time to complete healing in the study and control populations was 170.0 days (95% confidence interval [CI], 85.7–254.3) and 218.0 days (95% CI, 149.2–286.7) (log-rank, chi-square=3.99; p<0.046), respectively.
Conclusion
More than 20 weeks of HMB/Arg/Gln supplementation had a positive effect on difficult PU healing in older adults with multiple comorbidities. -
Citations
Citations to this article as recorded by- Impact of oral nutritional supplement composition on healing of different chronic wounds: A systematic review
Allan Carlos Soares do Espírito Santo, Clara Sandra de Araújo Sugizaki, Alcides Corrêa de Morais Junior, Nara Aline Costa, Maria Marcia Bachion, João Felipe Mota
Nutrition.2024; 124: 112449. CrossRef
- Impact of oral nutritional supplement composition on healing of different chronic wounds: A systematic review
- Association between dental amalgam restoration and urine mercury concentrations among young women: a cross-sectional study
- Su-Bin Park, Eun-Kyong Kim, Joon Sakong, Eun Young Park
- J Yeungnam Med Sci. 2023;40(4):373-380. Published online March 21, 2023
- DOI: https://doi.org/10.12701/jyms.2022.00955
- 1,095 View
- 57 Download
- 1 Web of Science
-
 Abstract
Abstract
 PDF
PDF - Background
The association between dental amalgam fillings and urine mercury concentrations was investigated in this study to assess the health risks associated with dental amalgams.
Methods
This cross-sectional study included 99 women in their 20s who visited the dental clinic in Daegu, Korea. The 99 participants were composed of 68 subjects who had dental amalgam fillings (exposure group) and 31 subjects who did not have dental amalgam fillings (nonexposure group). Oral examinations were conducted by a single dental hygienist, sociodemographic features were investigated as confounding variables, and urine mercury concentrations were measured using an automatic mercury analyzer.
Results
The mean±standard deviation of the urine mercury concentrations of the exposure and nonexposure groups were 1.50±1.78 μg/g creatinine and 0.53±0.63 μg/g creatinine, respectively. The exposure group showed significantly higher levels than the nonexposure group (p<0.01). The urine mercury concentration significantly increased with an increase in the number of teeth filled with amalgam, cavity surfaces involved, and number of defective amalgam fillings, and according to the latest exposure time (p<0.001). In the multiple regression analysis of amalgam-related factors and urine mercury concentrations after correction for confounding factors, the urine mercury concentration in the group with six or more amalgam-filled teeth, 11 or more cavity surfaces, and two or more defective amalgams was significantly higher than that in the nonexposure group (p<0.001).
Conclusion
According to this study, exposure to dental amalgams was confirmed to significantly affect urine mercury concentrations.
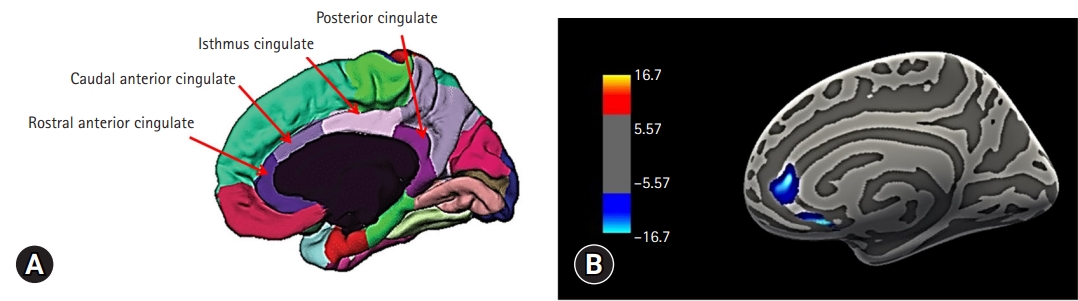
- Cortical thickness of the rostral anterior cingulate gyrus is associated with frailty in patients with end-stage renal disease undergoing hemodialysis in Korea: a cross-sectional study
- Sang Hyun Jung, Jong Soo Oh, So-Young Lee, Hye Yun Jeong
- J Yeungnam Med Sci. 2023;40(4):381-387. Published online March 24, 2023
- DOI: https://doi.org/10.12701/jyms.2022.00941
- 1,216 View
- 38 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Frailty is defined as a condition of being weak and delicate, and it represents a state of high vulnerability to adverse health outcomes. Recent studies have suggested that the cingulate gyrus is associated with frailty in the elderly population. However, few imaging studies have explored the relationship between frailty and the cingulate gyrus in patients with end-stage renal disease (ESRD) undergoing hemodialysis.
Methods
Eighteen right-handed patients with ESRD undergoing hemodialysis were enrolled in the study. We used the FreeSurfer software package to estimate the cortical thickness of the regions of interest, including the rostral anterior, caudal anterior, isthmus, and posterior cingulate gyri. The Beck Depression Inventory, Beck Anxiety Inventory, and laboratory tests were also conducted.
Results
The cortical thickness of the right rostral anterior cingulate gyrus (ACG) was significantly correlated with the Fried frailty index, age, and creatinine level. Multiple regression analysis indicated that the cortical thickness of the right rostral ACG was associated with frailty after controlling for age and creatinine level.
Conclusion
Our results indicate that the cortical thickness of the rostral ACG may be associated with frailty in patients with ESRD on hemodialysis and that the rostral ACG may play a role in the frailty mechanism of this population.
- Diagnostic value of serum procalcitonin and C-reactive protein in discriminating between bacterial and nonbacterial colitis: a retrospective study
- Jae Yong Lee, So Yeon Lee, Yoo Jin Lee, Jin Wook Lee, Jeong Seok Kim, Ju Yup Lee, Byoung Kuk Jang, Woo Jin Chung, Kwang Bum Cho, Jae Seok Hwang
- J Yeungnam Med Sci. 2023;40(4):388-393. Published online April 3, 2023
- DOI: https://doi.org/10.12701/jyms.2023.00059

- 1,253 View
- 54 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Differentiating between bacterial and nonbacterial colitis remains a challenge. We aimed to evaluate the value of serum procalcitonin (PCT) and C-reactive protein (CRP) in differentiating between bacterial and nonbacterial colitis.
Methods
Adult patients with three or more episodes of watery diarrhea and colitis symptoms within 14 days of a hospital visit were eligible for this study. The patients’ stool pathogen polymerase chain reaction (PCR) testing results, serum PCT levels, and serum CRP levels were analyzed retrospectively. Patients were divided into bacterial and nonbacterial colitis groups according to their PCR. The laboratory data were compared between the two groups. The area under the receiver operating characteristic curve (AUC) was used to evaluate diagnostic accuracy.
Results
In total, 636 patients were included; 186 in the bacterial colitis group and 450 in the nonbacterial colitis group. In the bacterial colitis group, Clostridium perfringens was the commonest pathogen (n=70), followed by Clostridium difficile toxin B (n=60). The AUC for PCT and CRP was 0.557 and 0.567, respectively, indicating poor discrimination. The sensitivity and specificity for diagnosing bacterial colitis were 54.8% and 52.6% for PCT, and 52.2% and 54.2% for CRP, respectively. Combining PCT and CRP measurements did not increase the discrimination performance (AUC, 0.522; 95% confidence interval, 0.474–0.571).
Conclusion
Neither PCT nor CRP helped discriminate bacterial colitis from nonbacterial colitis.
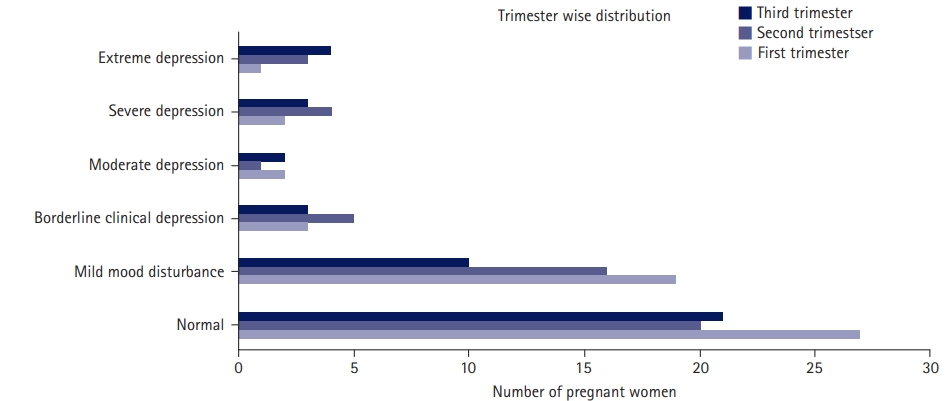
- Depression, sleep quality, and body image disturbances among pregnant women in India: a cross-sectional study
- Kranti S. Kadam, Aditya R. Anvekar, Vishnu B. Unnithan
- J Yeungnam Med Sci. 2023;40(4):394-401. Published online May 9, 2023
- DOI: https://doi.org/10.12701/jyms.2023.00087
- 1,212 View
- 70 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Pregnancy is associated with a number of physical, emotional, and biological changes that can exacerbate maternal psychological disturbances, such as body image concerns and depression. Sleep disturbances during pregnancy can also have adverse impacts. This study aimed to determine the prevalence of depression, sleep disturbances, and body image concerns among pregnant women. The study also examined the relationship between these factors and pregnancy-related variables, such as bad obstetric history and whether the pregnancies were unplanned.
Methods
A cross-sectional study of 146 pregnant patients was conducted at a tertiary care center over 15 months. The patients were administered the Beck Depression Inventory, Pittsburgh Sleep Quality Index, and Body Image Concern Inventory questionnaires. Contingency tables, Fisher exact test, and Spearman correlation were used to identify underlying relationships.
Results
The prevalence of depression was 22.6%. Although body image disturbance was noted in only 2.7% of patients, 46.6% had poor sleep quality. Poor sleep was associated with primigravida status. Bad obstetric history and unplanned pregnancy were associated with depression. Depression was found to be significantly correlated with body image disturbances and poor sleep quality.
Conclusion
Psychiatric disorders were prevalent during pregnancy. This study highlights the importance of screening for depression in pregnant patients. Counselling and caregiver education can be useful for mitigating psychological disturbances. Management of pregnancies by multidisciplinary teams that include psychiatrists could be immensely useful in improving the pregnancy experiences of patients.
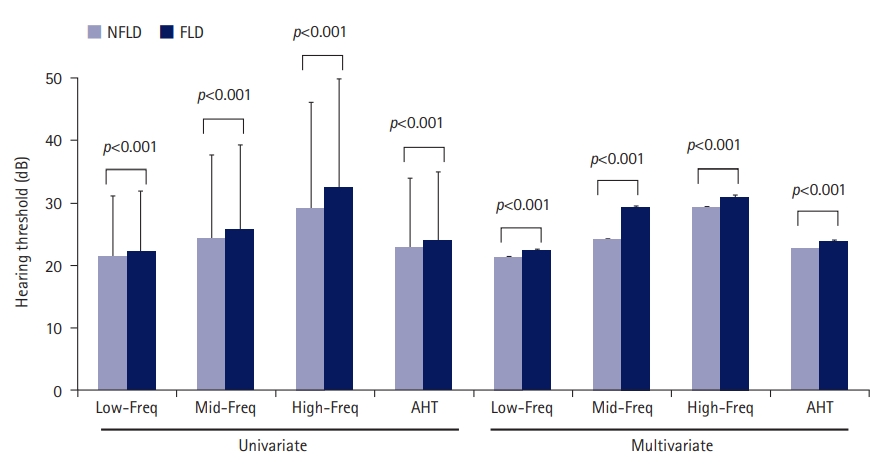
- Association between fatty liver disease and hearing impairment in Korean adults: a retrospective cross-sectional study
- Da Jung Jung
- J Yeungnam Med Sci. 2023;40(4):402-411. Published online June 26, 2023
- DOI: https://doi.org/10.12701/jyms.2023.00304
- 2,416 View
- 38 Download
-
 Abstract
Abstract
 PDF
PDF - Background
We hypothesized that fatty liver disease (FLD) is associated with a high prevalence of hearing loss (HL) owing to metabolic disturbances. This study aimed to evaluate the association between FLD and HL in a large sample of the Korean population.
Methods
We used a dataset of adults who underwent routine voluntary health checkups (n=21,316). Fatty liver index (FLI) was calculated using Bedogni’s equation. The patients were divided into two groups: the non-FLD (NFLD) group (n=18,518, FLI <60) and the FLD group (n=2,798, FLI ≥60). Hearing thresholds were measured using an automatic audiometer. The average hearing threshold (AHT) was calculated as the pure-tone average at four frequencies (0.5, 1, 2, and 3 kHz). HL was defined as an AHT of >40 dB.
Results
HL was observed in 1,370 (7.4%) and 238 patients (8.5%) in the NFLD and FLD groups, respectively (p=0.041). Compared with the NFLD group, the odds ratio for HL in the FLD group was 1.16 (p=0.040) and 1.46 (p<0.001) in univariate and multivariate logistic regression analyses, respectively. Linear regression analyses revealed that FLI was positively associated with AHT in both univariate and multivariate analyses. Analyses using a propensity score-matched cohort showed trends similar to those using the total cohort.
Conclusion
FLD and FLI were associated with poor hearing thresholds and HL. Therefore, active monitoring of hearing impairment in patients with FLD may be helpful for early diagnosis and treatment of HL in the general population.
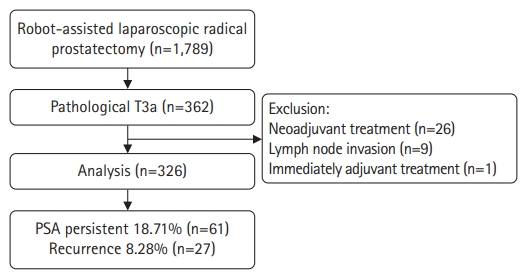
- Risk factors for prostate-specific antigen persistence in pT3aN0 prostate cancer after robot-assisted laparoscopic radical prostatectomy: a retrospective study
- Jun Seop Kim, Jae Hoon Chung, Wan Song, Minyong Kang, Hyun Hwan Sung, Hwang Gyun Jeon, Byong Change Jeong, Seong Il Seo, Hyun Moo Lee, Seong Soo Jeon
- J Yeungnam Med Sci. 2023;40(4):412-418. Published online June 28, 2023
- DOI: https://doi.org/10.12701/jyms.2023.00234
- 1,205 View
- 34 Download
-
 Abstract
Abstract
 PDF
PDF - Background
The aim of this study was to evaluate the risk factors for prostate-specific antigen (PSA) persistence in pathological stage T3aN0 prostate cancer (PCa) after robot-assisted laparoscopic radical prostatectomy (RALP).
Methods
A retrospective study was performed on 326 patients with pT3aN0 PCa who underwent RALP between March 2020 and February 2022. PSA persistence was defined as nadir PSA of >0.1 ng/mL after RALP, and the risk factors for PSA persistence were evaluated using logistic regression analysis.
Results
Among 326 patients, 61 (18.71%) had PSA persistence and 265 (81.29%) had PSA of <0.1 ng/mL after RALP (successful radical prostatectomy [RP] group). In the PSA persistence group, 51 patients (83.61%) received adjuvant treatment. Biochemical recurrence occurred in 27 patients (10.19%) in the successful RP group during the mean follow-up period of 15.22 months. Multivariate analysis showed that the risk factors for PSA persistence were large prostate volume (hazard ratio [HR], 1.017; 95% confidence interval [CI], 1.002–1.036; p=0.046), lymphovascular invasion (LVI) (HR, 2.605; 95% CI, 1.022–6.643; p=0.045), and surgical margin involvement (HR, 2.220; 95% CI, 1.110–4.438; p=0.024).
Conclusion
Adjuvant treatment may be needed for improved prognosis in patients with pT3aN0 PCa after RALP with a large prostate size, LVI, or surgical margin involvement.

 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine


 First
First Prev
Prev



