PubMed Central, CAS, DOAJ, KCI

Articles
- Page Path
- HOME > J Yeungnam Med Sci > Volume 41(2); 2024 > Article
-
Original article
Optimal examination for traumatic nerve/muscle injuries in earthquake survivors: a retrospective observational study -
Berkay Yalçınkaya
 , Büşranur Tüten Sağ
, Büşranur Tüten Sağ , Mahmud Fazıl Aksakal
, Mahmud Fazıl Aksakal , Pelin Analay, MD
, Pelin Analay, MD , Hasan Ocak
, Hasan Ocak , Murat Kara
, Murat Kara , Bayram Kaymak
, Bayram Kaymak , Levent Özçakar
, Levent Özçakar
-
Journal of Yeungnam Medical Science 2024;41(2):120-127.
DOI: https://doi.org/10.12701/jyms.2024.00087
Published online: April 5, 2024
Department of Physical and Rehabilitation Medicine, Hacettepe University Medical School, Ankara, Turkey
- Corresponding author: Berkay Yalçınkaya, MD Department of Physical and Rehabilitation Medicine, Hacettepe University Medical School, Hacettepe Üniversitesi Tıp Fakültesi Hastaneleri, Zemin Kat FTR AD, Sıhhıye, Ankara 06230, Turkey Tel: +90-312-305-1080 • E-mail: berkay0lka@gmail.com
© 2024 Yeungnam University College of Medicine, Yeungnam University Institute of Medical Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 494 Views
- 23 Download
Abstract
-
Background
- Physiatrists are facing with survivors from disasters in both the acute and chronic phases of muscle and nerve injuries. Similar to many other clinical conditions, neuromusculoskeletal ultrasound can play a key role in the management of such cases (with various muscle/nerve injuries) as well. Accordingly, in this article, a recent single-center experience after the Turkey-Syria earthquake will be rendered.
-
Methods
- Ultrasound examinations were performed for various nerve/muscle lesions in 52 earthquake victims referred from different cities. Demographic features, type of injuries, and applied treatment procedures as well as detailed ultrasonographic findings are illustrated.
-
Results
- Of the 52 patients, 19 had incomplete peripheral nerve lesions of the brachial plexus (n=4), lumbosacral plexus (n=1), and upper and lower limbs (n=14).
-
Conclusion
- The ultrasonographic approach during disaster relief is paramount as regards subacute and chronic phases of rehabilitation. Considering technological advances (e.g., portable machines), the use of on-site ultrasound examination in the (very) early phases of disaster response also needs to be on the agenda of medical personnel.
- Natural disasters are unexpected occurrences that can result in destruction and heavy casualties [1,2], and earthquakes are likely to have the greatest negative impact on human health among them. Growing populations have increased the need for living spaces, especially in cities, thereby putting individuals in a riskier position against earthquakes in developing countries. On February 6, 2023, two earthquakes (moment magnitudes of 7.8 and 7.6) with a 9-hour interval struck southern Turkey and western Syria. At present, they are the strongest “doublet” earthquakes ever recorded in the Levant [3]. The impact on mortality (fifth deadliest of the 21st century) and costs (fourth costliest) was catastrophic [4]. As an interesting side note, the occurrence of these earthquakes in this region is also believed to be a sign of the apocalypse. Likewise, the great battle (Armageddon) is also expected to take place in this zone.
- From a medical perspective, physicians need to tackle various neuromusculoskeletal conditions and their complications (e.g., fracture, crush injury, amputation, compartment syndrome, and nerve lesions) after earthquakes. In addition to the well-established role of physiatrists in the long-term rehabilitation of pertinent cases, the medical services provided to these patients can notably be upgraded with the prompt and convenient use of ultrasound (US) examination. US can play a key role in diagnosing soft tissue and peripheral nerve lesions in posttraumatic conditions. Some exemplary findings would include focal nerve/fascicular enlargement, loss of internal fascicular structure, nerve discontinuity, and increased cross-sectional area of the nerve in nerve injuries [5]. Traumatic muscles can show signs of swelling with or without focal/general areas of increased echogenicity (muscle strain), hypo/hyperechogenic appearance with or without fibrillar discontinuity (muscle contusion), hypoechoic or anechoic circumscribed lesions (muscle hematoma), and muscle atrophy [6,7]. Sono-Tinel, a probe compression that causes pain on the pathological side, is also suggestive of these lesions [8]. To this end, also being aware of the mounting utility of US in physiatry, we considered that a pictorial essay summarizing our recent experience with the Kahramanmaraş earthquake would help to exemplify its actual contribution to disaster relief. In particular, we tried to render how US examination impacted our medical approach to nerve/muscle injuries.
Introduction
- Ethical statements: Patient consent was obtained from the patients before the physical examination. An approval from the Institutional Review Board was waived due to the retrospective nature of the study.
- Hacettepe University Hospital is a tertiary referral center that has treated earthquake survivors. A total of 52 individuals—who were consulted from different in-patient services or who applied to our outpatient clinic—were examined. Table 1 summarizes the clinical features and treatment methods used. Earthquake survivors who had been examined in our department between February 13, 2023 and April 4, 2023 were included, and pertinent data were collected between April 5, 2023 and April 29, 2023.
- After a complete physical examination (orthopedic examination of all involved joints and their adjacent joints and neurological examination including muscle strength, light touch sensation, pain sensation, deep tendon reflexes, and pathological reflex examinations), all patients were also evaluated for various nerve/muscle injuries by US examination. Six patients were scanned using a 5 to 12 MHz linear transducer (GE Logiq P5, Madison, WI, USA), and a portable device with a linear transducer (4–13 MHz, Clarius L7; Clarius Mobile Health, Vancouver, BC, Canada) was used for the remaining cases.
Methods
- The mean age of the patients was 29.4±19.4 years (range, 7–72 years). The mean duration of being trapped under rubble was 28.6±30.4 hours (range, 4–120 hours). Nineteen patients had peripheral nerve involvement, including four brachial plexuses, one lumbosacral plexus, and 17 limb nerve injuries (the peroneal nerve being the most affected) (Table 1). The characteristic ultrasonographic findings of earthquake victims with nerve/muscle injuries are summarized in Table 2. Electrodiagnostic studies were not performed because the patients had skin lesions such as abrasion and edema or were bandaged. Magnetic resonance imaging (MRI) for plexopathy was performed in five patients. The remaining patients were diagnosed with peripheral nerve entrapment based on physical and ultrasonographic examinations. Of the 52 patients, six who had demonstrative/exemplary imaging findings were selected for this study. They are further discussed in detail, with a special focus on the US findings.
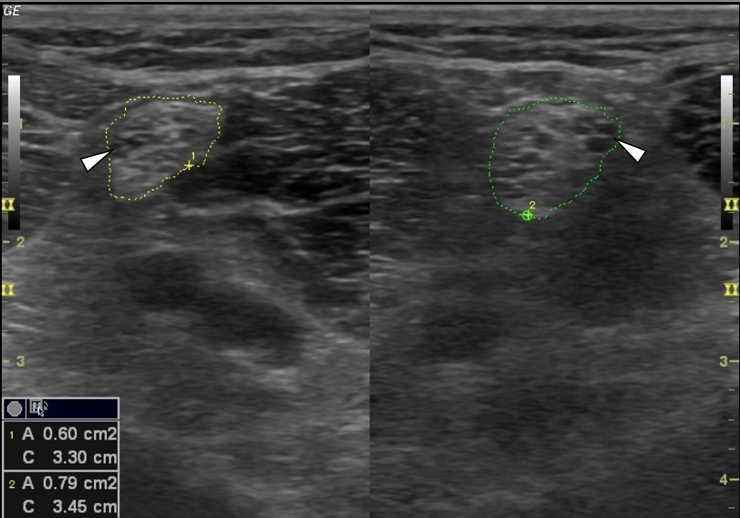
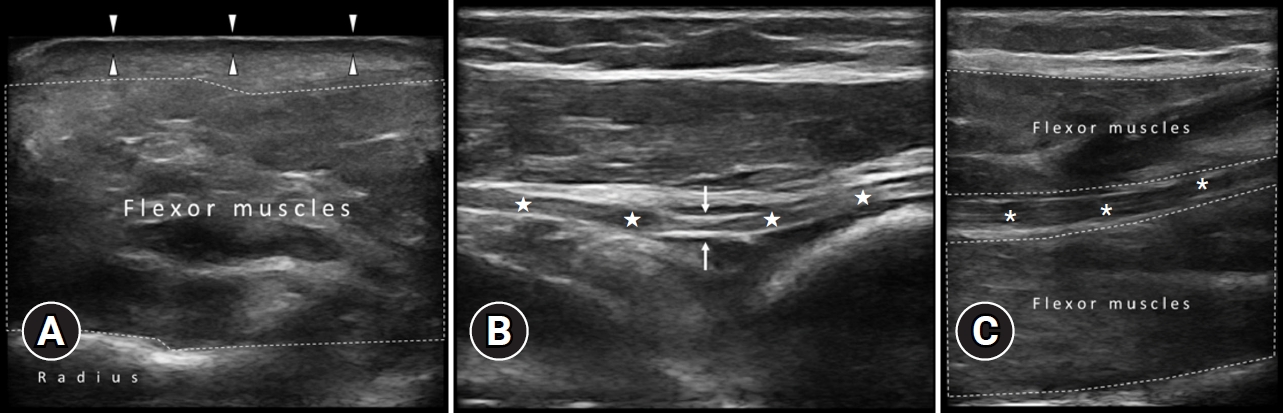
- 1. Case 1
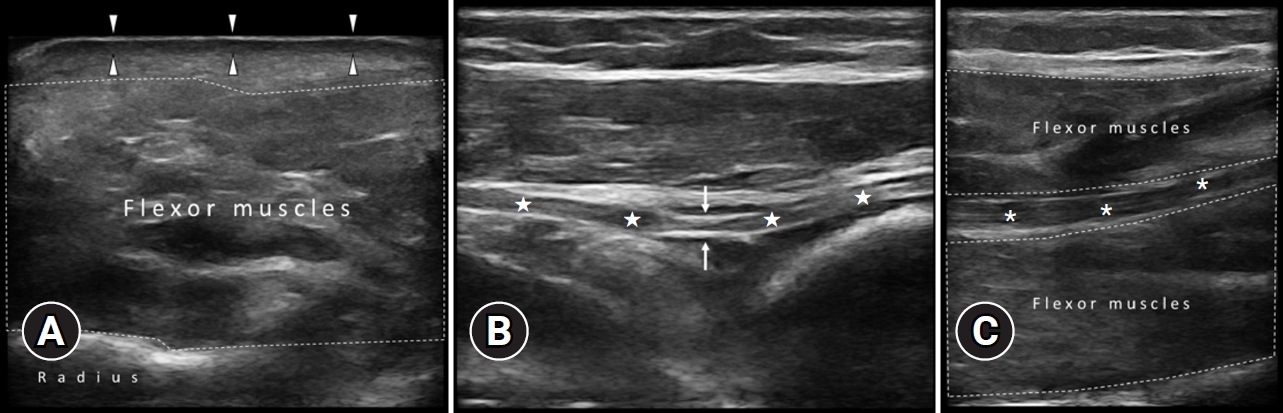
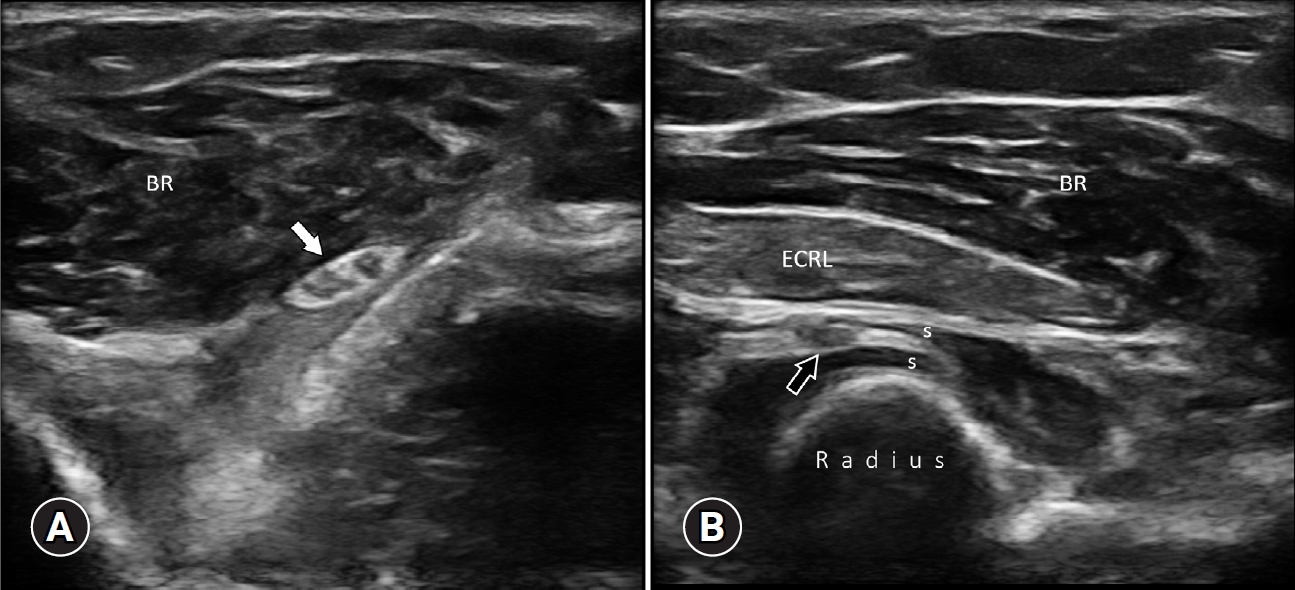
- A 53-year-old female with left transfemoral amputation. She was trapped under rubble for 56 hours, and her leg was pinned under a steel door. Although she had no motor deficits, she had sensory loss on the dorsal side of her right hand and hypoesthesia in all fingers (median greater than the ulnar side). She had also multiple abrasions on her right forehand. US examination of the forearm/elbow revealed dermal/subcutaneous edema and heterogeneous hypo/hyperechoic flexor muscles. US also showed a swollen posterior interosseous nerve (PIN) with proximal and distal compression sites and a swollen median nerve in the mid-forearm. The superficial radial nerve (SRN) was edematous, particularly underneath the scarred area (Figs. 1, 2; Supplementary Videos 1–5). Based on the physical and US examinations, the patient was diagnosed with median, PIN, and SRN neuropathies.
- 2. Case 2
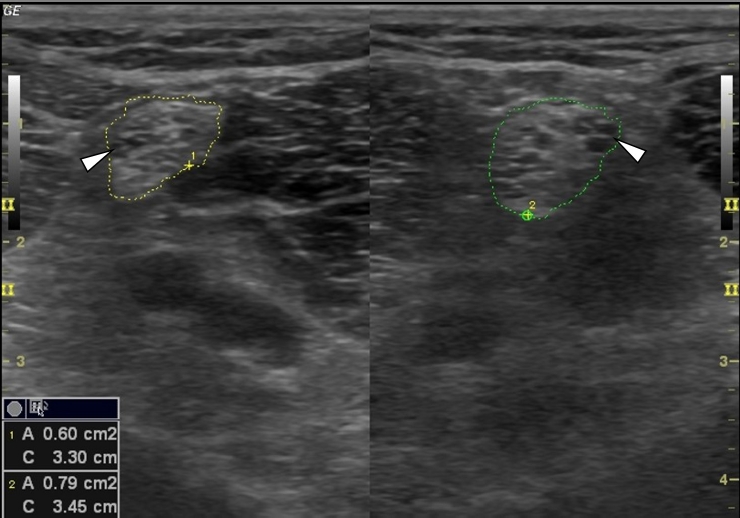
- A 51-year-old female with right transhumeral amputation. She was trapped under rubble for 32 hours. Physical examination revealed weak left shoulder abductors, elbow flexors, and extensors (1+/5, 0/5, and 2/5, respectively). Wrist flexors, extensors, and hand intrinsic muscles were also weak on the left side (4–/5). She described hypoesthesia on an area innervated by the C5 nerve root. Deep tendon reflexes were negative. US examination of the brachial plexus at the interscalene region revealed swollen nerve roots (especially C5) compared with the normal side (Fig. 3). MRI of the brachial plexus was compatible with C5 to C7 nerve root involvement. Based on the physical examination and imaging findings, the patient was diagnosed with brachial plexopathy.
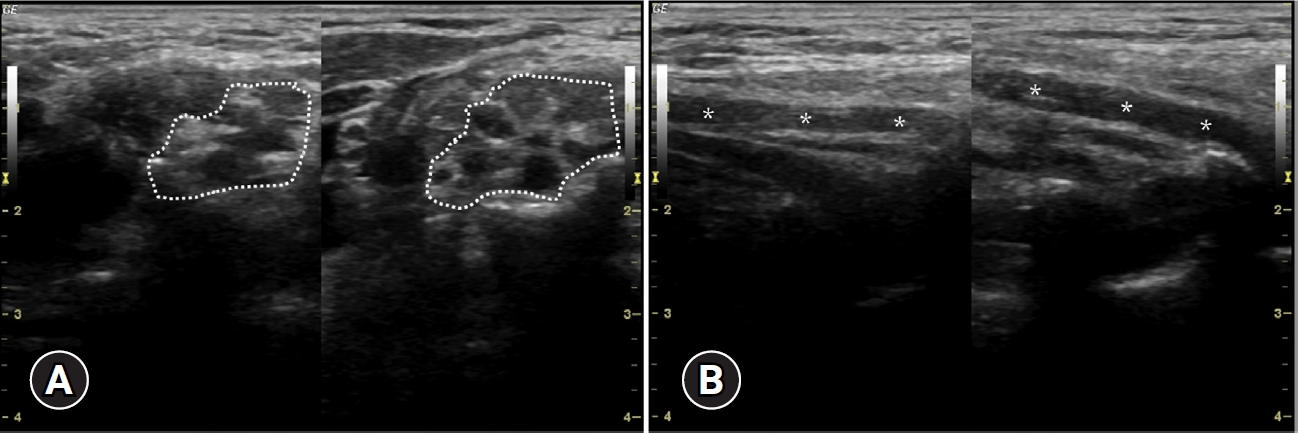
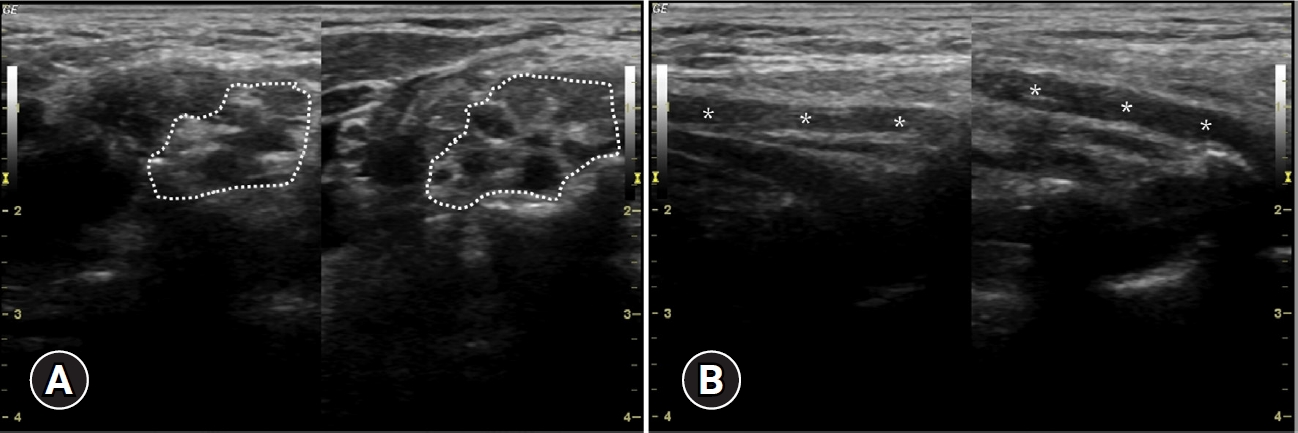
- 3. Case 3
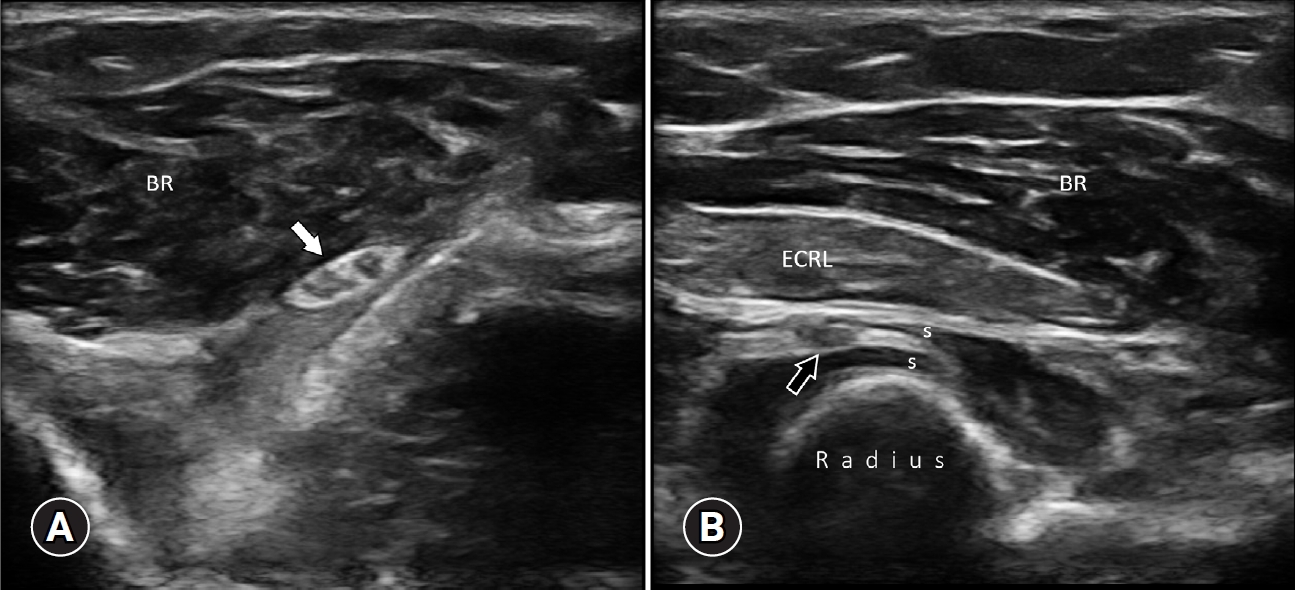
- A 33-year-old female with wrist drop. She was trapped under rubble for 6 hours. She also had a talus fracture. On physical examination, the wrist and finger extensors were weak (3–/5 and 1/5, respectively) and the rest of the neurological examination was normal. US examination of the distal arm and proximal forearm depicted an edematous radial nerve and PIN (Fig. 4, Supplementary Video 6). The patient was diagnosed with radial nerve and PIN involvement based on the physical examination and US findings.
- 4. Case 4
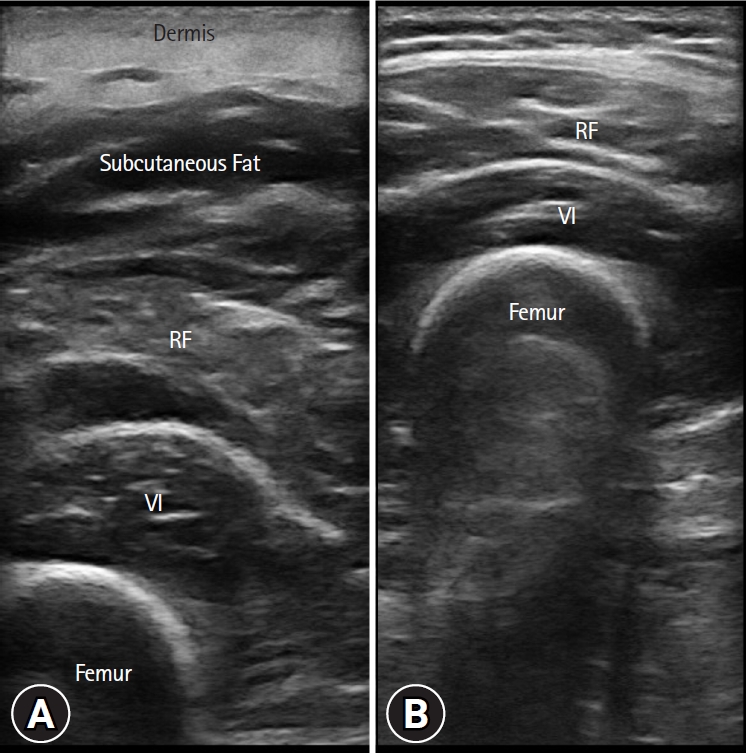
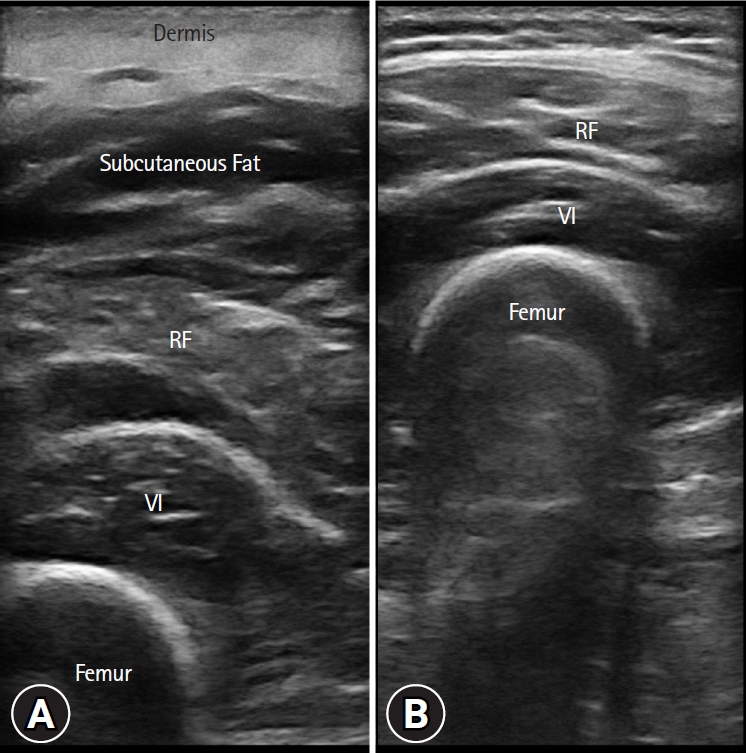
- A 15-year-old male with a painful left hip/leg. He was trapped under rubble for 6 hours. Due to severe hip pain, he tended to keep his left leg always in the same position (i.e., flexion, abduction, and external rotation). On physical examination, hip adduction and internal rotation were limited. His left leg was also painful upon palpation. Neurological examinations were otherwise noncontributory. US examination of the anterior hip region revealed a hematoma in the iliopsoas muscle. The dermis, subcutaneous fat, rectus femoris, and vastus intermedius muscles were swollen in the left thigh (Fig. 5, Supplementary Videos 7–10). These findings were consistent with early strain in the anterior thigh muscles.
- 5. Case 5
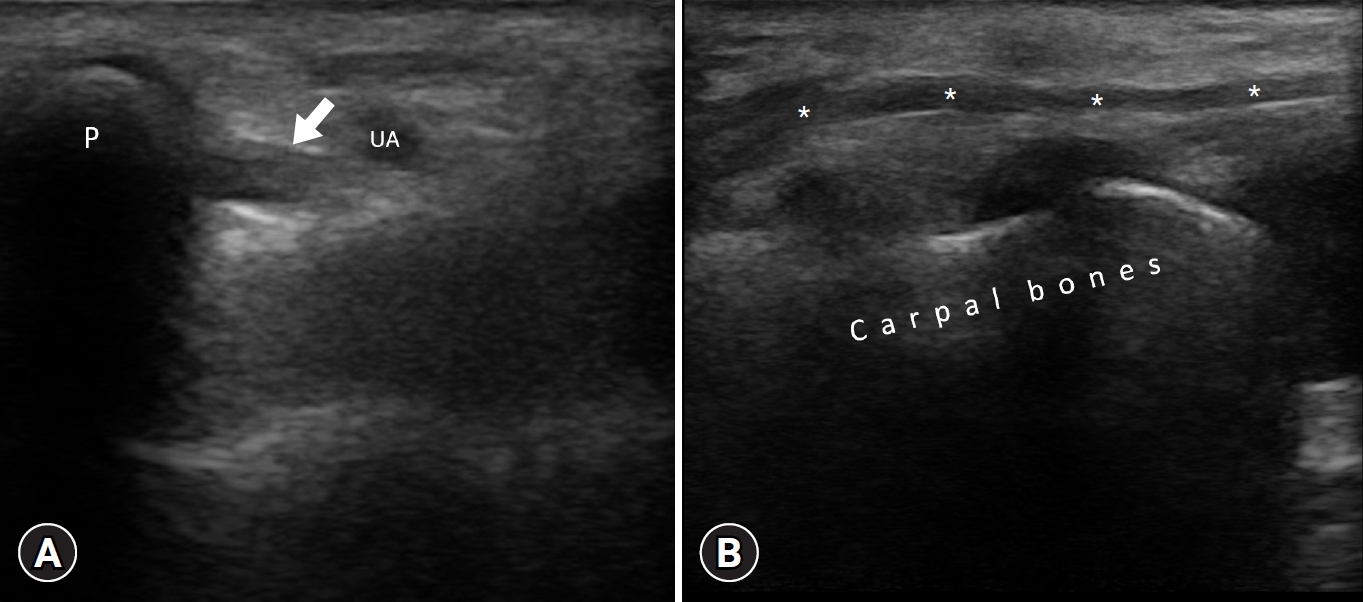
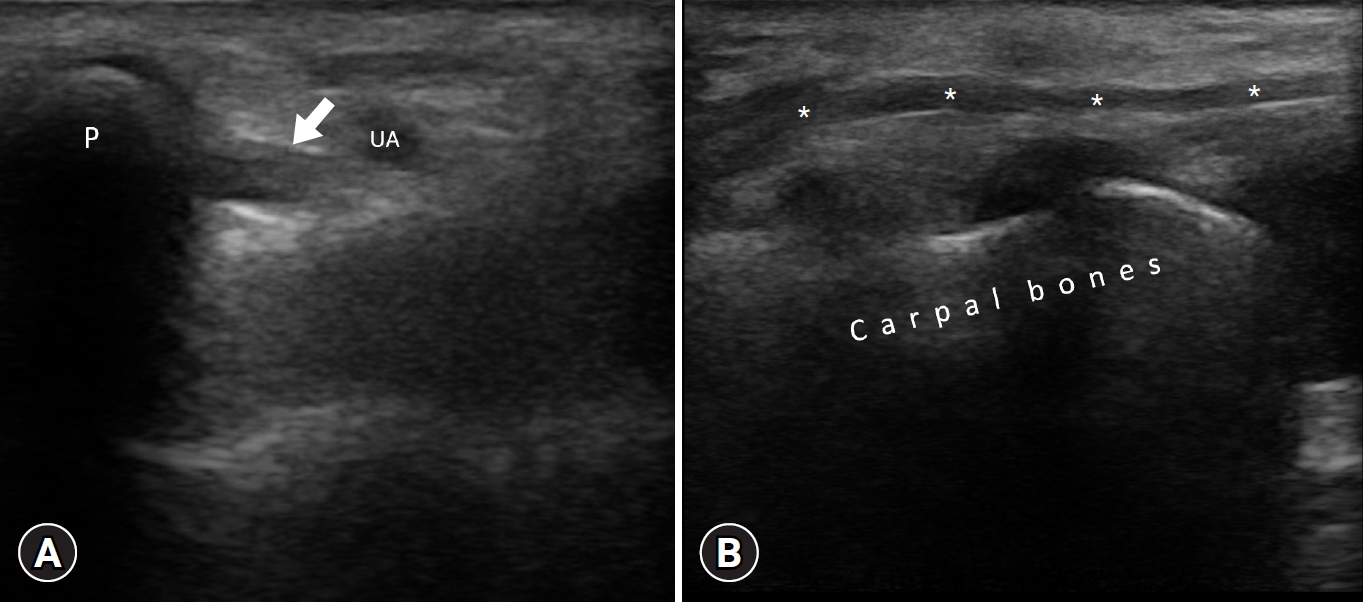
- A 16-year-old female with right transhumeral amputation. She was trapped under rubble for 80 hours. On inspection, she had a claw hand on her left side. The 3rd and 4th lumbrical muscle strength was 2/5, and the abductor digiti minimi muscle strength was 1/5. She had hypoesthesia in her 4th and 5th fingers. The rest of the neurological examination was unremarkable. US examination showed an edematous ulnar nerve passing through Guyon’s canal (Fig. 6). Based on the physical and US examinations, the patient was diagnosed with ulnar neuropathy. Supplementary Video 11 shows an edematous ulnar nerve in another patient.
- 6. Case 6
- An 18-year-old male with bilateral foot drop. He was trapped under rubble for 36 hours. On physical examination, foot dorsiflexors and plantar flexors were weak (0/5) on both sides. He also described hypoesthesia on the dorsal/plantar side of the right foot. US examination revealed fascicular edema in both sciatic nerves (Fig. 7, Supplementary Video 12). Based on physical and US examinations, the patient was diagnosed with bilateral sciatic neuropathy. Supplementary Videos 13 and 14 show swollen peroneal nerves in another patient with a similar history.
Results
- US is a simple, fast, and inexpensive examination method that plays an important role in the management of traumatic peripheral nerve/muscle injuries [9,10]. Owing to its portability, not only in routine daily practice but also in several settings can it be applied in a convenient/effective way. Following our recent experience, we actually aim to extend the possibility―also to include its use “on-site.” In other words, physiatrists/physicians would be capable of contributing to the prompt triage of these patients. Needless to say, the spectrum of emergency pathologies that can be examined with US also comprises those of the cortical bone. As such, occult fractures can also be diagnosed simultaneously. Indeed, these fractures may be associated with lesions in the surrounding peripheral nerves or soft tissues/muscles. Discontinuity of the hyperechoic cortical bone and hypoechoic subperiosteal hematoma are the major US findings in bone fractures in the acute phase [11].
- Peripheral nerves can be injured by mechanical compression, ischemia, or direct trauma [12]. While the diagnosis can already be challenging enough in daily routine, an earthquake scenario definitely adds up to the difficulty of diagnosis. Yet, the complexity of the trauma (compartment syndrome, fasciotomy, fractures, amputation, etc.) and the accompanying medical conditions would contribute to this aspect. Additionally, electrodiagnosis is either impossible or has limited use in these patients. Of note, the other (magnetic resonance) imaging option is again not applicable for several simple reasons. On the contrary, the flexible use of the US transducer provides access to different regions regardless of the patient’s position/condition. Scanning throughout their entire course, peripheral nerves as well as the pertinent muscles can be examined both statically and dynamically, where appropriate. Nerve integrity, edema, partial/complete rupture, and the underlying cause of injury are examined in a comprehensive approach. In the management of earthquake survivors, US plays a paramount role in ensuring early and accurate diagnosis, facilitating the timely initiation of appropriate rehabilitation program, it encompasses a spectrum of interventions, including range of motion, strengthening and mobilization exercises where applicable, functional electrical stimulation of denervated muscles, orthoses/splints, prosthetic programs for patients with amputated limbs, and various physical therapy modalities for pain control [13]. US will also assist in the prompt implementation of tailored rehabilitation plans during follow-up. It is noteworthy that the patient-friendly nature of US indisputably helps the physician and the “already traumatized” patient alike. After precise diagnoses, physical therapy, interventions, or surgery can timely be applied. Lastly, US will also aid in closely monitoring the morphological changes during healing/treatment.
Discussion
-
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
-
Funding
None.
-
Author contributions
Conceptualization, Resources, Visualization: all authors; Formal analysis, Supervision: LÖ; Methodology: MK, BK, LÖ; Investigation: BY, BTS, MK, BK, LÖ; Writing-original draft: BY, MK, BK, LÖ; Writing-review & editing: MK, BK, LÖ.
Article information
Supplementary materials
Supplementary Video 1.
Supplementary Video 2.
Supplementary Video 3.
Supplementary Video 4.
Supplementary Video 5.
Supplementary Video 6.
Supplementary Video 7.
Supplementary Video 8.
Supplementary Video 9.
Supplementary Video 10.
Supplementary Video 11.
Supplementary Video 12.
Supplementary Video 13.
Supplementary Video 14.

| Site | Finding |
|---|---|
| Nerve | Increased cross-sectional area |
| Fascicular edema | |
| Nerve compression | |
| Focal nerve enlargement | |
| Plexopathy | |
| Muscle | Muscle strain |
| Muscle contusion | |
| Muscle hematoma |
- 1. Khan F, Amatya B, Gosney J, Rathore FA, Burkle FM Jr. Medical rehabilitation in natural disasters: a review. Arch Phys Med Rehabil 2015;96:1709–27.ArticlePubMed
- 2. Amatya B, Galea M, Li J, Khan F. Medical rehabilitation in disaster relief: towards a new perspective. J Rehabil Med 2017;49:620–8.ArticlePubMed
- 3. Dal Zilio L, Ampuero JP. Earthquake doublet in Turkey and Syria. Commun Earth Environ 2023;4:71.Article
- 4. Wikipedia contributors. 2023 Turkey-Syria earthquake [Internet]. Wikipedia, The Free Encyclopedia; 2023 Apr 26 [cited 2024 Jan 25]. https://en.wikipedia.org/w/index.php?title=2023_Turkey%E2%80%93Syria_earthquake&oldid=1151836296.
- 5. Ricci V, Ricci C, Cocco G, Gervasoni F, Donati D, Farì G, et al. Histopathology and high-resolution ultrasound imaging for peripheral nerve (injuries). J Neurol 2022;269:3663–75.ArticlePubMedPDF
- 6. Chang KV, Wu WT, Özçakar L. Ultrasound ımaging and rehabilitation of muscle disorders: Part 1. Traumatic ınjuries. Am J Phys Med Rehabil 2019;98:1133–41.ArticlePubMed
- 7. Feger J, Bell D. Muscle contusion [Internet]. Radiopaedia.org; [cited 2024 Mar 7]. https://doi.org/10.53347/rID-82383.Article
- 8. Ricci V, Özçakar L. Life after ultrasound: are we speaking the same (or a new) language in Physical and Rehabilitation Medicine? J Rehabil Med 2019;51:234–5.ArticlePubMed
- 9. Özçakar L, Ricci V, Chang KV, Mezian K, Kara M. Musculoskeletal ultrasonography: ninety-nine reasons for physiatrists. Med Ultrason 2022;24:137–9.ArticlePubMedPDF
- 10. Baloch N, Hasan OH, Jessar MM, Hattori S, Yamada S. “Sports Ultrasound”, advantages, indications and limitations in upper and lower limbs musculoskeletal disorders: review article. Int J Surg 2018;54(Pt B):333–40.ArticlePubMed
- 11. Cocco G, Ricci V, Villani M, Delli Pizzi A, Izzi J, Mastandrea M, et al. Ultrasound imaging of bone fractures. Insights Imaging 2022;13:189.ArticlePubMedPMCPDF
- 12. Menorca RM, Fussell TS, Elfar JC. Nerve physiology: mechanisms of injury and recovery. Hand Clin 2013;29:317–30.ArticlePubMedPMC
- 13. Rathore FA, Gosney JE, Reinhardt JD, Haig AJ, Li J, DeLisa JA. Medical rehabilitation after natural disasters: why, when, and how? Arch Phys Med Rehabil 2012;93:1875–81.ArticlePubMed
References
Figure & Data
References
Citations

- Figure
- Related articles
-
- Association between fatty liver disease and hearing impairment in Korean adults: a retrospective cross-sectional study
- Preemptive pyloroplasty for iatrogenic vagus nerve injury in intrahepatic cholangiocarcinoma patients undergoing extensive left-sided lymph node dissection: a retrospective observational study
- Assessment of normal anal sphincter anatomy using transanal ultrasonography in healthy Korean volunteers: a retrospective observational study
- Clinical investigation on acute pyelonephritis without pyuria: a retrospective observational study

 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine PubReader
PubReader ePub Link
ePub Link Cite
Cite