PubMed Central, CAS, DOAJ, KCI

Articles
- Page Path
- HOME > J Yeungnam Med Sci > Volume 40(2); 2023 > Article
-
Original article
Outcomes after repair of complete atrioventricular canal with a modified single-patch technique: a retrospective study -
George Samanidis1,2
 , Konstantinos Kostopanagiotou3
, Konstantinos Kostopanagiotou3 , Meletios Kanakis2
, Meletios Kanakis2 , Georgios Kourelis4
, Georgios Kourelis4 , Kyriaki Kolovou5
, Kyriaki Kolovou5 , Georgios Vagenakis6, Dimitrios Bobos2, Nicholas Giannopoulos2
, Georgios Vagenakis6, Dimitrios Bobos2, Nicholas Giannopoulos2 -
Journal of Yeungnam Medical Science 2023;40(2):187-192.
DOI: https://doi.org/10.12701/jyms.2022.00759
Published online: February 1, 2023
1Department of Adult Cardiac Surgery, Onassis Cardiac Surgery Center, Athens, Greece
2Department of Paediatric and Congenital Heart Surgery, Onassis Cardiac Surgery Center, Athens, Greece
3Department of Thoracic Surgery, Attikon University Hospital of Athens, Athens, Greece
4Paediatric Cardiac and Adult Congenital Heart Disease Intensive Care Unit, Onassis Cardiac Surgery Center, Athens, Greece
5Department of Cardiac Surgery Intensive Care, Onassis Cardiac Surgery Center, Athens, Greece
6Department of Paediatric Cardiology and Adult Congenital Heart Disease, Onassis Cardiac Surgery Center, Athens, Greece
- Corresponding author: George Samanidis, MD, PhD Department of Adult Cardiac Surgery, Onassis Cardiac Surgery Center, 356 Leoforos Syggrou, Athens 17674, Greece Tel: +30-21-0949-3833 • E-mail: gsamanidis@yahoo.gr
Copyright © 2023 Yeungnam University College of Medicine, Yeungnam University Institute of Medical Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,309 Views
- 53 Download
Abstract
-
Background
- This study aimed to present the short- and midterm outcomes after complete atrioventricular canal defect (CAVC) repair using a single-patch technique.
-
Methods
- This study included 30 children who underwent surgical correction of the CAVC using a single-patch technique.
-
Results
- The median age of the patients was 5.7 months (interquartile range [IQR], 5.0–7.5 months), and 23 patients (76.7%) had type A CAVC. Fourteen patients (46.7%) were female and 17 (56.7%) had been diagnosed with Down syndrome. The in-hospital mortality rate was 0%. No deaths were observed during a median follow-up of 4 years (IQR, 3.5–5.0 years). Patients without Down syndrome were associated with late moderate mitral regurgitation (MR) (p=0.02). Late MR less than moderate degree was observed in 96.6%, 78.5%, and 50% of patients after 2, 4, and 5 years of follow-up, respectively, while late tricuspid valve regurgitation less than moderate degree was observed in 96.7%, 85.9%, and 59.0% of patients after 2, 4, and 6 years of follow-up, respectively. After a median follow-up of 4 years, only one patient had required surgical repair of a left ventricular outflow tract obstruction, which occurred 26 months after the first operation. Multivariable logistic regression analysis adjusted for the type of CAVC, sex, Down syndrome, age, and weight revealed that the absence of Down syndrome was a risk factor for late moderate MR (MR-2) (odds ratio, 0.05; 95% confidence interval, 0.006–0.50; p=0.01).
-
Conclusion
- A single-patch technique for CAVC surgical repair is a safe method with acceptable short- and midterm results.
- Atrioventricular (AV) septal defects include a spectrum of cardiac malformations characterized by varying degrees of incomplete development of the inferior portion of the atrial septum, inflow portion of the ventricular septum, and AV valves. This group of defects can be further subdivided into partial, intermediate, and complete forms. In the complete AV canal (CAVC) form of AV septal defects, the key element is the presence of a single AV valve that is common to the right and left AV chambers. The central aspect of this orifice is usually contiguous, with an ostium primum type of atrial septal defect above and a defect in the ventricular septum below [1]. Rastelli et al. [2] classified complete AV septal defects into types A, B, and C and highlighted the variable degree of bridging by the left superior leaflet in a continuous spectrum of leaflet and chordal anatomies. Since the first successful repair of a complete AV septal defect by Lillehei in 1955, three different techniques have been employed. The modified single-patch technique was introduced by Wilcox et al. [3] and Nicholson et al. [4]. All techniques (double-patch, single-patch, and modified single-patch) are in use today; but, until now, there has been no comparison between them. Comparing outcomes between the modified single-patch and double-patch surgical techniques seem difficult since the disease is heterogeneous and rare, and the surgeon may have a preference for the technique used. Although the double-patch technique seems to be a more thorough anatomical repair, the modified single-patch technique has an easier and faster learning curve, and uses a simplified approach [5,6].
- Patients with repaired CAVCs represent a substantial percentage of grown-up congenital heart disease cases, and the efficacy of these techniques has been verified over the years. Herein, we present the midterm results from one center after CAVC repair using the modified single-patch technique.
Introduction
- Ethical statements: The study was performed in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study was approved by the Institutional Review Board and Ethics Committee of Onassis Cardiac Surgery Center (No. 705/15.01.2021). Informed consent for surgery was obtained preoperatively from the relatives of the children.
- 1. Study population
- The study included 30 children who underwent CAVC repair using the single-patch technique from 2015 to 2022 in a single cardiac surgery center. The surgical procedure was performed by three surgeons. All patients were preoperatively evaluated by a cardiologist and transthoracic echocardiography (TTE). The classification of CAVC was based on the Rastelli classification [2]. Type B CAVC was not observed in any patient. All perioperative and follow-up data were recorded in our database. Postoperative length of stay in the intensive care unit and in the hospital was recorded.
- The patients were followed up in the outpatient clinic with routine clinical examinations and TTE. ΤΤΕ was performed during the hospital stay, 1 week after hospital discharge, and every 6 months thereafter. AV valve function postoperative and at follow-up was evaluated using TTE. The last follow-up date was the date when TTE was performed. Currently, there are no clear criteria for grading mitral regurgitation (MR) in children. New echocardiographic indices and classification systems for semiquantitative and quantitative evaluations have been proposed for adults; however, their validity and reproducibility in children are unknown. Quantitative assessment is often important to guide the management of children with MR [7]. Postoperative MR and tricuspid valve regurgitation (TR) were initially classified as follows: without, mild, moderate, and severe [7]. Furthermore, for the purpose of this study and data analysis, the postoperative and follow-up MR and TR were divided into two groups based on degree (trivial-to-mild regurgitation MR and mild-to-moderate regurgitation MR). MR-1 and TR-1 were defined before discharge, while MR-2 and TR-2 were defined at follow-up.
- 2. Surgical technique
- All patients underwent midline sternotomy. In cases of previous pulmonary artery banding (PAB), redo midline sternotomy was performed. Fresh pericardium was used in all cases. Standard aortic and bicaval venous cannulation was performed by placing the patient on cardiopulmonary bypass with the superior vena cava cannula first. A vent was placed in the left heart through the right superior pulmonary vein. The patient was cooled to 34°C. Histidine-tryptophan-ketoglutarate solution was used for cardioplegia. The modified single-patch technique was used in all cases [1,3,4]. In cases where PAB had caused pulmonary artery stricture, pulmonary artery plasty was also performed using a piece of bovine pericardium. In one case, the sternum was left open after leaving the theater and was closed the next day uneventfully.
- 3. Statistical analysis
- Continuous variables are presented as median (interquartile range [IQR]) and the rest as number (percentage). The normality of variable distribution was tested using the Shapiro-Wilk test, histograms, and Q-Q plots. The Student t-test, Mann-Whitney test, chi-square test, or Fisher exact test were used for data analysis. Correlations between variables were examined using Spearman (rs) or Pearson (r) correlation coefficients. Binary logistic regression analysis was implemented to identify the possible risk factors for postoperative MR and TR, and the effect size was presented as the odds ratio (OR). The confidence interval (CI) was set at 95%. Statistically significant differences were considered if p<0.05. IBM SPSS ver. 25 for Windows (IBM Corp., Armonk, NY, USA) was used for data analysis.
Methods
- Of the 30 patients who underwent surgery, 23 (76.7%) had type A CAVC. The median age of the patients was 5.7 months (IQR, 5.0–7.5 months). There were 14 female patients (46.7%) and 17 patients (56.7%) with Down syndrome (trisomy 21). None of the patients had other genetic abnormalities. Regarding defect size, the ventricular component ranged from 12 to 16 mm, and the atrial component ranged from 11 to 21 mm. Previous PAB was recorded in six patients (20.0%). The median aortic cross-clamp (ACC) time was 92 minutes (IQR, 74–105 minutes). Other perioperative details are listed in Table 1. No difference in cardiopulmonary bypass and ACC times was observed between patients with and without previous PAB (p>0.05 for both; t-test and Mann-Whitney test, respectively) (Table 2). Postoperative MR-1 (mild-to-moderate) and TR-1 (mild-to-moderate) were not associated with the type of CAVC, previous PAB, sex, or presence of trisomy 21 (all p>0.05) (Table 3). In addition, patient age and weight at the time of surgery were not associated with MR-1 and TR-1 (all p>0.05) (Table 3). In contrast, patient weight at the time of surgery was closely associated with TR-1 (p=0.06), while age was not (p=0.27) (Table 3). In two cases, postoperative chylothorax was observed, which was treated medically. The median in-hospital length of stay was 8 days (IQR, 7–9 days), while the 30-day mortality and in-hospital mortality were both 0%. Early or late pacemaker implantation was not required in any patient.
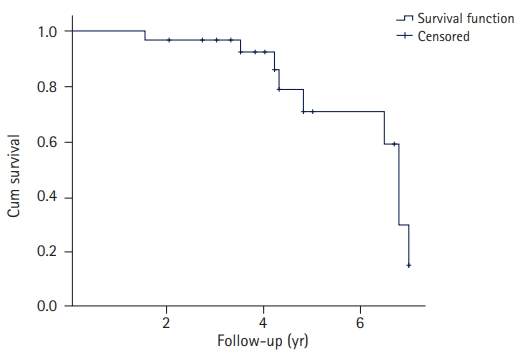
- The median follow-up of patients was 48 months (IQR, 42–60 months). No deaths were observed during follow-up. The degree of AV valve regurgitation during follow-up was recorded by TTE. The follow-up TTE findings and data are presented in Table 4. The type of CAVC and sex were not associated with late moderate MR-2 (p>0.05), while not having trisomy 21 was associated with late moderate MR-2 (p=0.02, Fisher exact test) (Table 5). The type of CAVC, sex, and trisomy 21 was not associated with late moderate TR-2 (p>0.05, Fisher exact test) (Table 5). In addition, age and weight at the date of surgery were not associated with late moderate MR-2 and TR-2 (p>0.05, Mann-Whitney test) (Table 5). Left ventricular outflow tract (LVOT) obstruction was observed in one patient 26 months after surgery. During follow-up, MR less than moderate degree was observed in 96.6%, 78.5%, and 50% of patients at 2, 4, and 5 years, respectively (Fig. 1), while TR less than moderate degree was observed in 96.7%, 85.9%, and 59% of patients at 2, 4, and 6 years, respectively (Fig. 2). After a median follow-up of 4 years, one patient had undergone surgery for LVOT obstruction 26 months after the first operation. Multivariable logistic regression analysis adjusted for type of CAVC, sex, Down syndrome, age, and weight revealed that the absence of trisomy 21 was a risk factor for late moderate MR (MR-2) (OR, 0.05; 95% CI, 0.006–0.50; p=0.01) (Table 6).
Results
- The modified single-patch repair technique for CAVC is a well-established technique [5-8,9]. However, division of the bridging leaflets is often required, and this process may cause some issues during the long-term follow-up of these patients. Nevertheless, survival rates after CAVC repair with the modified single-patch technique have been reported to be 98.8%, 96.3%, and 96.3% at 5, 10, and, 20 years, respectively [5,10]. Our intermediate results indicated a mortality rate of 0%. Our patients were children and experienced an excellent quality of life.
- AV valve function during follow-up, especially the left AV valve, has always been an issue, and the modified single-patch technique has been associated with this complication [5]. However, in a large study, moderate regurgitation of the left AV valve was reported in 15% of patients, and that finding did not correlate with trisomy 21, history of PAB, cleft management, or age [5]. Freedom from reoperation for left AV valve regurgitation has been reported to be as low as 62% after 10 years [11]. Reynen et al. [5] described reoperation for left AV valve regurgitation in 6% of cases. Most investigators did not find any relationship between left AV valve regurgitation and trisomy 21 [5]. Backer et al. [12] performed a meta-analysis of the three repair techniques and found that the rate of reoperation for left AV valve regurgitation was 2% in the modified single-patch, 7% in the two-patch, and 9.7% in the classic single-patch technique. In our study, moderate left AV valve regurgitation was observed in 23.3% of patients, but none of them required left AV valve reintervention. In addition, in our study, there was no requirement for pacemaker implantation as a postoperative procedure. Pacemaker reoperations have been described in patients previously, varying between 2% and 12% [10,13].
- LVOT obstruction is a well-described mid- to long-term complication of CAVC repair [14]. In 4% to 5% of patients, LVOT obstruction may require reoperation. In our study, one patient required reoperation for LVOT obstruction, which was diagnosed 2 years after initial repair. The pathology was consistent with the development of a discrete subaortic membrane, and reoperation was successfully performed. During the latest follow-up, the patient was free of recurrence.
- This study was a retrospective analysis of patients who underwent CAVC correction using the modified single-patch technique. The small number of patients in this study may have affected our analysis (short-, mid-, and long-term results). Furthermore, the patients underwent surgery in a single department of a tertiary Cardiac Surgery Hospital. This study included only infants and children. In addition, the study did not include a comparison of the two techniques (single- versus double-patch technique) to draw reliable conclusions about the effectiveness and benefits of the single-patch technique.
- The single-patch technique for CAVC surgical repair is a method with acceptable short- and midterm results considering that it is a simplified approach. However, long-term assessment is warranted, and prospective randomized studies are needed to compare the advantages and disadvantages between the double-patch and modified single-patch techniques.
Discussion
-
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
-
Funding
None.
-
Author contributions
Conceptualization, Investigation: GS, MK, GK, K Kolovou, GV, DB, NG; Data curation, Formal analysis, Methodology, Visualization, Validation: GS, MK; Resources: GS; Supervision: MK; Writing-original draft: GS, K Kostopanagiotou, MK, GK, K Kolovou, GV, NG; Writing-review & editing: GS.
Notes
| Variable |
Previous pulmonary artery banding |
p-value | |
|---|---|---|---|
| Yes | No | ||
| Cardiopulmonary bypass time (min) | 110.0±22.0 | 120.6±20.0 | 0.30 |
| Aortic cross-clamp time (min) | 78.0 (72.0–90.0) | 93.5 (82.0–105.0) | 0.32 |
| Variable |
MR at follow-up |
TR at follow-up |
||||
|---|---|---|---|---|---|---|
| No (n=17) | Yes (n=13) | p-value | No (n=21) | Yes (n=9) | p-value | |
| Type of CAVC | 0.10 | >0.99 | ||||
| A | 11 | 12 | 16 | 7 | ||
| C | 6 | 1 | 5 | 2 | ||
| Female sex | 8 | 6 | >0.99 | 9 | 5 | 0.69 |
| Down syndrome | 13 | 4 | 0.02* | 13 | 4 | 0.44 |
| Age (mo) | 6.0 (5.5–6.5) | 5.5 (5.0–9.0) | 0.99 | 6.0 (5.0–9.0) | 5.5 (5.2–6.0) | 0.26 |
| Weight (kg) | 6.8 (5.8–7.8) | 7.1 (6.8–8.2) | 0.78 | 7.1 (6–8.2) | 5.8 (5.8–6.3) | 0.06 |
| Variable | OR (95% CI) | p-value |
|---|---|---|
| Type of CAVC, C | 0.05 (0.003–1.26) | 0.07 |
| Female sex | 1.03 (0.08–11.90) | 0.98 |
| Down syndrome | 0.05 (0.006–0.49) | 0.01* |
| Age | 0.92 (0.36–2.39) | 0.87 |
| Weight | 1.51 (0.42–5.48) | 0.52 |
- 1. Pacifico AD. Atrio-ventricular septal defects. In: Stark JF, de Leval MR, Tsang VT, editors. Surgery for congenital heart defects. 3rd ed. Chichester, UK; Hoboken, NJ: John Wiley & Sons; 2006.
- 2. Rastelli G, Kirklin JW, Titus JL. Anatomic observations on complete form of persistent common atrioventricular canal with special reference to atrioventricular valves. Mayo Clin Proc 1966;41:296–308.PubMed
- 3. Wilcox BR, Jones DR, Frantz EG, Brink LW, Henry GW, Mill MR, et al. Anatomically sound, simplified approach to repair of "complete" atrioventricular septal defect. Ann Thorac Surg 1997;64:487–94.ArticlePubMed
- 4. Nicholson IA, Nunn GR, Sholler GF, Hawker RE, Cooper SG, Lau KC, et al. Simplified single patch technique for the repair of atrioventricular septal defect. J Thorac Cardiovasc Surg 1999;118:642–6.ArticlePubMed
- 5. Reynen S, Hövels-Gürich HH, Vazquez-Jimenez JF, Messmer BJ, Sachweh JS. Long-term outcome up to 40 years after single patch repair of complete atrioventricular septal defect in infancy or childhood. Thorac Cardiovasc Surg 2021;69(Suppl 3):e68–75.ArticlePubMedPMC
- 6. Stephens EH, Backer CL. Teaching the modified single-patch technique for complete atrioventricular septal defect. World J Pediatr Congenit Heart Surg 2022;13:371–5.ArticlePubMedPDF
- 7. Cantinotti M, Giordano R, Koestenberger M, Voges I, Santoro G, Franchi E, et al. Echocardiographic examination of mitral valve abnormalities in the paediatric population: current practices. Cardiol Young 2020;30:1–11.ArticlePubMed
- 8. Geoffrion TR, Singappuli K, Murala JSK. A review of the Nunn modified single patch technique for atrioventricular septal defect repair. Transl Pediatr 2018;7:91–103.ArticlePubMedPMC
- 9. Azzab S, Samy A, Singab H, Zeinah M, Musollari G, Axiaq A, et al. The effect of surgical technique, age, and trisomy 21 on early outcome of surgical management of complete atrioventricular canal defect. Cardiol Young 2022;32:869–73.ArticlePubMed
- 10. Ginde S, Lam J, Hill GD, Cohen S, Woods RK, Mitchell ME, et al. Long-term outcomes after surgical repair of complete atrioventricular septal defect. J Thorac Cardiovasc Surg 2015;150:369–74.PubMed
- 11. Houck CA, Evertz R, Teuwen CP, Roos-Hesselink JW, Kammeraad JA, Duijnhouwer AL, et al. Dysrhythmias in patients with a complete atrioventricular septal defect: from surgery to early adulthood. Congenit Heart Dis 2019;14:280–7.ArticlePubMedPDF
- 12. Backer CL, Kaushal S, Mavroudis C. Modified single-patch technique: repairing complete atrioventricular septal defect. Ann Pediatr Cardiol 2009;2:51–4.ArticlePubMedPMC
- 13. Di Mambro C, Calvieri C, Silvetti MS, Tamburri I, Giannico S, Baban A, et al. Bradyarrhythmias in repaired atrioventricular septal defects: single-center experience based on 34 years of follow-up of 522 patients. Pediatr Cardiol 2018;39:1590–7.ArticlePubMedPDF
- 14. Backer CL, Eltayeb O, Mongé MC, Wurlitzer KC, Hack MA, Boles LH, et al. Modified single patch: are we still worried about subaortic stenosis? Ann Thorac Surg 2015;99:1671–6.ArticlePubMed
References
Figure & Data
References
Citations


 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine
 PubReader
PubReader ePub Link
ePub Link Cite
Cite



