Ultrasound imaging and guidance in the management of myofascial pain syndrome: a narrative review
Article information
Abstract
Myofascial pain syndrome (MPS) is a common musculoskeletal disorder characterized by muscle pain, tenderness, and trigger points. Ultrasonography has emerged as a key tool for diagnosing and treating MPS owing to its ability to provide precise, minimally invasive guidance. This review discusses the use of ultrasonography in various approaches to evaluate and manage MPS. Studies have shown that shear-wave sonoelastography can effectively assess muscle elasticity and offer insights into trapezius stiffness in patients with MPS. Ultrasound-guided interfascial hydrodissection, especially with visual feedback, has demonstrated effectiveness in treating trapezius MPS. Similarly, ultrasound-guided rhomboid interfascial plane blocks and perimysium dissection for posterior shoulder MPS have significantly reduced pain and improved quality of life. The combination of extracorporeal shockwave therapy with ultrasound-guided lidocaine injections has been particularly successful in reducing pain and stiffness in trapezius MPS. Research regarding various guided injections, including dry needling, interfascial plane blocks, and fascial hydrodissection, emphasizes the importance of ultrasonography for accuracy and safety. Additionally, ultrasound-guided delivery of local anesthetics and steroids to the quadratus lumborum muscle has shown lasting pain relief over a 6-month period. Overall, these findings highlight the pivotal role of ultrasonography in the assessment and treatment of MPS.
Introduction
Myofascial pain syndrome (MPS) is a common musculoskeletal disorder characterized by localized muscle pain and tenderness and is often associated with trigger points and hyperirritable spots within the muscle tissue or fascia [1]. MPS is estimated to affect up to 85% of the general population depending on the specific diagnostic criteria and population studied [2]. MPS can significantly affect an individual’s quality of life (QOL), limit mobility, and contribute to chronic pain. The mechanisms underlying MPS are complex and not yet fully understood. Trigger points are believed to form because of sustained muscle contraction or stress, leading to localized ischemia and the release of inflammatory mediators [3]. This cascade results in increased sensitization of nociceptors, contributing to localized and referred pain. Common factors that lead to the development of MPS include muscle overuse, trauma, poor posture, and stress. MPS can occur in various regions of the body; however, some areas are more prone to developing trigger points. These include the upper trapezius, levator scapulae, rhomboids, quadratus lumborum, and infraspinatus [4]. These muscles are often involved in maintaining posture and are susceptible to repetitive strain injury.
Ultrasonography (US) has emerged as a valuable tool for assessing MPS, allowing clinicians to visualize muscle tissue and detect changes in the echotexture, which may indicate the presence of trigger points. Grayscale US can identify alterations in the muscle architecture, whereas sonoelastography can measure tissue stiffness, potentially highlighting areas of increased tension [5]. This noninvasive technique provides real-time imaging, enabling a detailed assessment of muscle structure without radiation exposure. US guidance is increasingly used in the treatment of MPS [6]. It facilitates precise needle placement for various interventions, such as trigger point injections, interfascial hydrodissection (IH), and nerve hydrodissection [7]. These targeted treatments can reduce pain and improve function. Additionally, US guidance enhances the safety and accuracy of these procedures by allowing clinicians to visualize the surrounding structures and avoid complications. Considering the wide utility of US for musculoskeletal disorders, this review article discusses US imaging and guidance for the assessment and management of MPS.
Literature search
A systematic method was used to identify relevant research articles. Literature searches were conducted using four electronic databases: PubMed, Scopus, Embase, and Web of Science. The search timeframe was from the establishment of each database through April 1, 2024. The search terms used were “myofascial pain”, “trigger point”, “ultrasound”, and “sonography”. The inclusion criteria were as follows: (1) studies involving human subjects and (2) studies utilizing US for either the assessment or guided treatment of MPS. The exclusion criteria were as follows: (1) studies involving nonhuman subjects, (2) studies using imaging methods other than US for MPS evaluation and guided treatment, (3) studies without measurable clinical outcome data, and (4) studies that did not focus on patients with MPS.
Using the search strategy outlined above, we identified several key topics for further exploration, including (1) sonoelastography for MPS of the upper trapezius, (2) US-guided IH for MPS of the trapezius and the effect of visual feedback, (3) US-guided rhomboid interfascial plane block for rhomboid MPS, (4) US-guided perimysium dissection for posterior shoulder MPS, (5) combined therapy for trapezius MPS with shockwave and lidocaine injection, (6) various injection targets for MPS, and (7) US-guided delivery of local anesthetics and steroids for quadratus lumborum MPS. A summary of the included studies is presented in Table 1.
Sonoelastography for myofascial pain syndrome of the upper trapezius
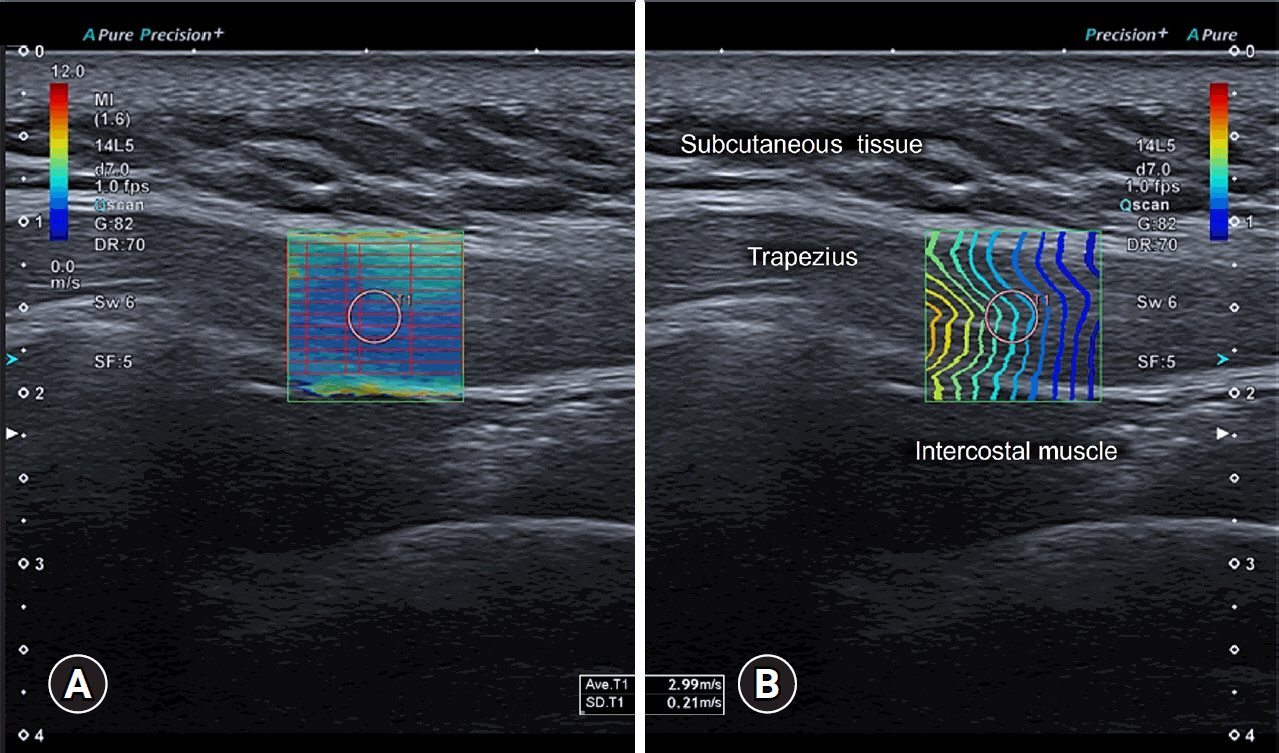
In 2023, Hao et al. [5] presented the findings of a prospective study involving the sequential enrollment of 109 patients with right posterior neck pain. Among them, 51 were diagnosed with MPS, whereas the remaining 58 were diagnosed with non-MPS-related neck discomfort. Real-time shear-wave elastography (SWE) was used to assess the mean shear-wave velocity (mSWV) of the right trapezius, with the measuring point established at the midpoint between the foramen magnum and the end of the right acromion (Fig. 1). Significantly elevated trapezius mSWV values were observed in patients with MPS compared with the values in their non-MPS counterparts. Stratified analysis based on pain severity indicated comparable trapezius mSWV values between individuals with mild pain and those without MPS. However, individuals with moderate and severe pain in the MPS group exhibited higher mSWV values than those in the non-MPS group. The area under the curve (AUC) value for the upper trapezius mSWV in patients with MPS was 0.791, with corresponding sensitivity and specificity values of 86.27% and 62.07%, respectively. Further subgroup analysis by pain severity yielded AUC values for the trapezius mSWV in patients with MPS with mild, moderate, and severe pain of 0.578, 0.899, and 0.983, respectively. This study identified increased stiffness in the trapezius muscle of patients with cervical MPS with moderate and severe pain. mSWV, which reflects trapezius muscle elasticity, may hold substantial value in the effective screening of cervical MPS, particularly in patients experiencing moderate and severe pain.
Ultrasonography-guided interfascial hydrodissection for trapezius myofascial pain syndrome and the effect of visual feedback
In 2023, Suarez-Ramos et al. [8] conducted a randomized controlled trial to investigate the immediate and prolonged effects of ultrasound-guided IH, utilizing 2% lidocaine and saline solution, in comparison with dry needling (DN) for managing MPS affecting the upper trapezius muscle. This single-blind study employed IH with an in-plane approach, in which a combination of 1 mL of 2% lidocaine and 5 mL of saline was injected between the fascia of the trapezius muscle and the underlying fascia using US guidance (Fig. 2). Both study groups were instructed to perform daily self-stretching exercises (SSE) after the procedure. Pain levels were assessed using the visual analog scale (VAS), and QOL was measured using the EuroQol 5-Dimension 5-Level (EQ-5D-5L) questionnaire. Blinded assessments were conducted before the intervention, immediately after the intervention, and at various intervals for up to 6 months. The study involved 46 participants with two dropouts, and both groups displayed significant variations in VAS scores over time. The IH+SSE group exhibited a more pronounced effect than the DN+SSE group. Although no statistically significant differences were found in the EQ-5D-5L dimensions, a greater effect size was observed for improvement in usual activities, pain/discomfort, and anxiety/depression. The authors concluded that IH is an effective technique for addressing both short- and long-term symptoms of MPS, offering an alternative strategy for individuals with chronic MPS in the upper trapezius.
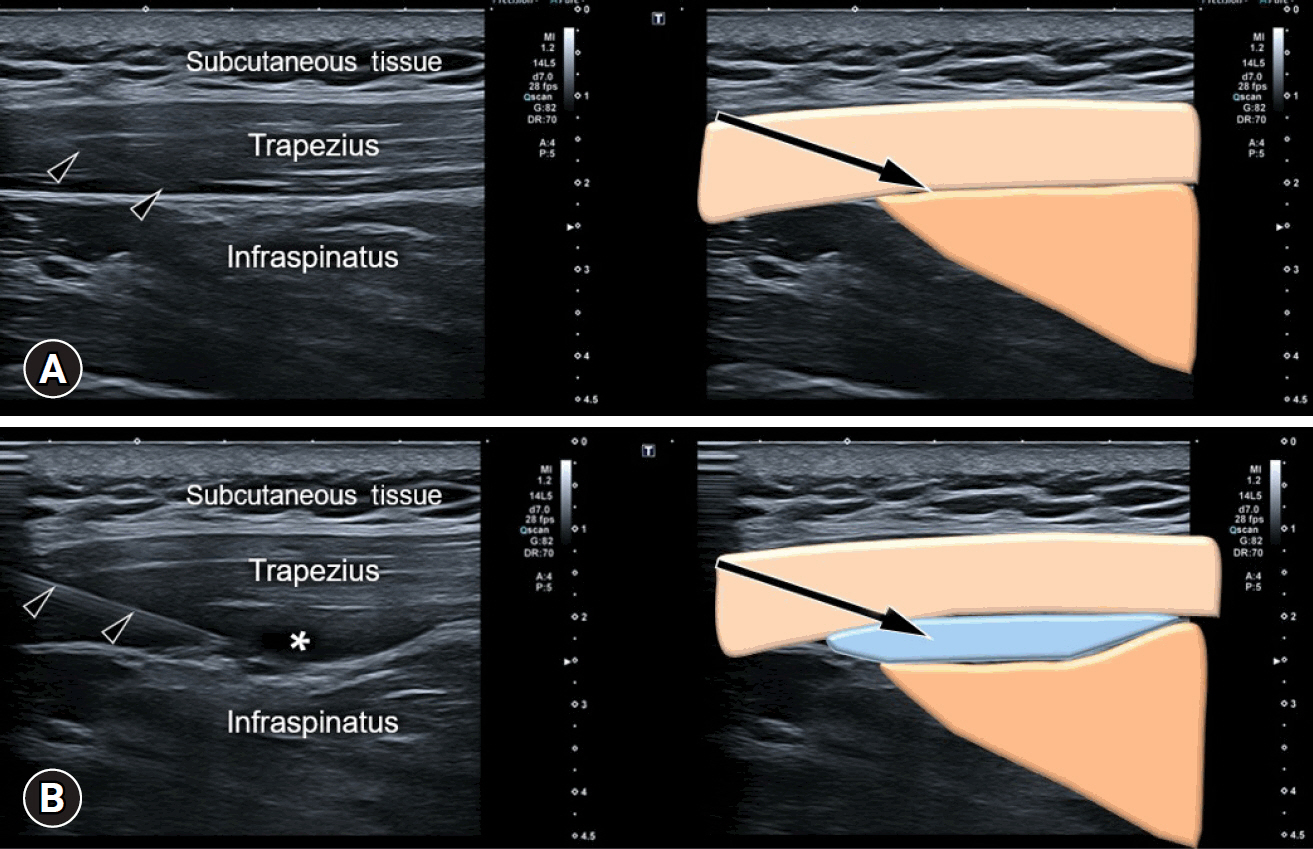
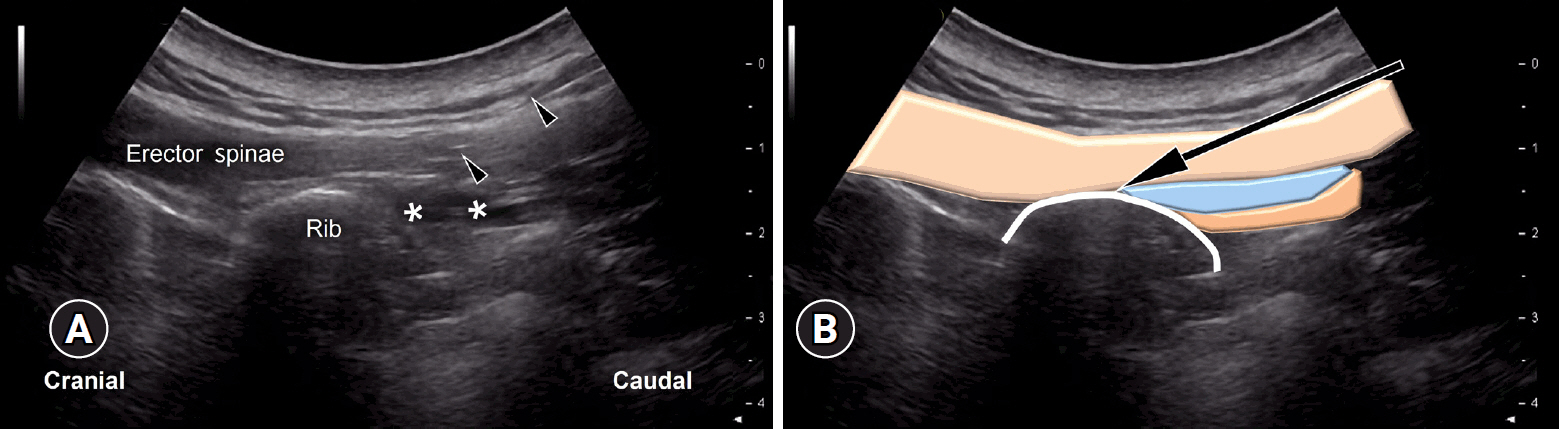
Ultrasound imaging (left side) and schematic drawing (right side) of ultrasound-guided interfascial hydrodissection of the trapezius muscle: (A) before and (B) after administering the injectant. The arrowheads indicate the needle trajectory, while the asterisk marks the injectant. The arrows represent the needle trajectory.
In 2022, Hasuo et al. [9] conducted an exploratory clinical trial to examine the influence of visual feedback following ultrasound-guided hydrodissection on treatment expectations and its potential association with pain reduction. The primary outcome was the numeric rating scale (NRS), which assessed treatment expectations immediately after hydrodissection, comparing outcomes between groups with and without visual feedback. A total of 136 outpatients underwent ultrasound-guided hydrodissection for MPS. The group that received visual feedback displayed significantly higher treatment expectations immediately after hydrodissection than the nonvisual feedback group. These heightened expectations were sustained on day 14 after the treatment. Prior to hydrodissection, the NRS scores for treatment expectations were comparable in both groups; however, a substantial increase was observed in the visual feedback group immediately after the procedure. Additionally, on day 14, the visual feedback group demonstrated a 67.7% improvement in NRS pain scores by 50% or more, compared with a 36.6% improvement in the nonvisual feedback group. Further analysis revealed that visual feedback played a pivotal role in the reduction in NRS pain scores at 14 days, which was indirectly mediated by the augmentation of treatment expectations. In summary, the use of visual feedback during US-guided hydrodissection emerged as a factor that enhanced treatment expectations immediately after the procedure, potentially contributing to reduced pain in individuals with MPS.
Ultrasonography-guided interfascial plane block for rhomboid myofascial pain syndrome
In 2023, Ozyemisci Taskiran et al. [10] conducted a retrospective study to investigate the immediate and enduring effects of ultrasound-guided rhomboid interfascial plane block in alleviating pain severity, reducing disability, and enhancing the QOL among patients with MPS characterized by trigger points in the rhomboid muscle. Participants diagnosed with MPS, having endured pain for at least 3 months with a severity rating of at least 4/10 on the NRS and having trigger points in the rhomboid muscle, underwent US-guided interfascial plane block. Needle insertion precisely targeted the underlying fascia of the rhomboid muscle over the ribs at the most tender point (Fig. 3). Adhering to maximum dose recommendations (2 mg/kg [0.8 mL/kg] of bupivacaine 0.25% with a maximum total amount of 175 mg [70 mL]), approximately 20 mL of bupivacaine 0.25% was administered via an in-plane technique in a 45° caudocranial direction using a 22-gauge 50-mm US-visible peripheral nerve block needle. Pain intensity, the self-reported neck pain and disability scale, and the Nottingham Health Profile were evaluated pretreatment and 1 week, 1 month, and 1 year after injection. The study enrolled 23 participants, revealing statistically significant reductions in pain severity in approximately 90%, 60% to 70%, and 50% of the patients at 1 week, 1 month, and 1 year after injection, respectively. Disability scores significantly improved in 70% and 56% of patients at the 1-month and 1-year follow-ups, respectively. Enhanced QOL was observed at the 1-month follow-up and sustained at the 1-year follow-up. These findings indicate that rhomboid interfascial plane block could serve as an effective long-term treatment option for MPS, contributing to the alleviation of pain and disability, improvement in QOL, and overall patient satisfaction.
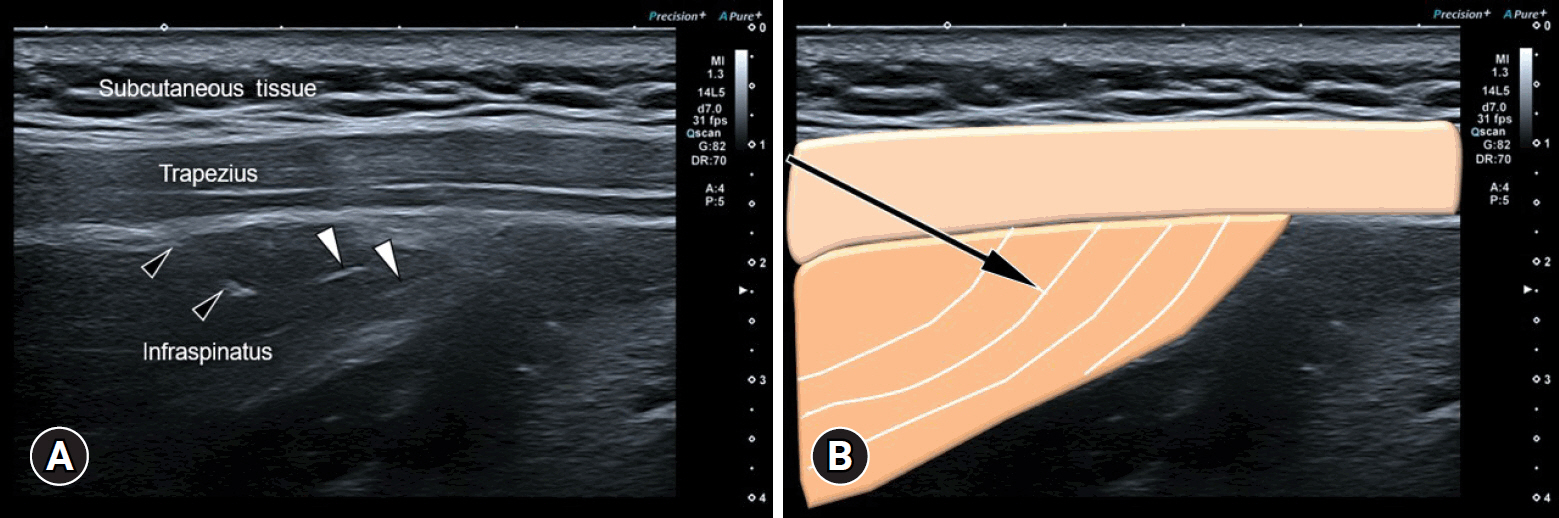
Ultrasonography-guided perimysium dissection for posterior shoulder myofascial pain syndrome
In 2021, Lai et al. [11] conducted a retrospective single-arm study to evaluate the efficacy and safety of perimysium dissection in refractory chronic myofascial pain of the posterior shoulder. Fifty-seven patients with this condition underwent perimysium dissection with US guidance. Under visualization, a 70-mm long 23-gauge needle attached to a 10-mL syringe was used to inject dextrose solution into the targeted perimysium, achieving a layered dissection over the infraspinatus or teres minor muscles (Fig. 4). VAS scores and complication rates were assessed before and 4 weeks after the procedure. Perimysium dissection with dextrose solution demonstrated excellent treatment efficacy and safety. After treatment, 33.3% of the participants were pain-free and 56.1% experienced over 50% improvement in pain scores. Among those with complete VAS records, the overall mean pre- and posttreatment VAS scores were 7.18±1.60 and 1.91±2.04, respectively, showing significant improvement in both infraspinatus and teres minor MPS subgroups. No complications were reported, except in one participant who received retreatment for teres minor MPS. The investigators concluded that US-guided perimysium dissection is a straightforward, safe, and effective injection method for managing posterior myofascial shoulder pain.
Combined therapy for upper trapezius myofascial pain syndrome with shockwave and lidocaine injection
In 2022, Anwar et al. [12] published a randomized controlled trial in which participants were randomly assigned to shockwave, shockwave and US-guided trigger point injection (combined), and control groups. The evaluation utilized diverse metrics, including VAS, neck disability index, electromyography, infrared thermography, and sonoelastography at baseline and at 1-week and 4-week intervals. The upper trapezius trigger points were identified with a 13 to 6 MHz linear transducer, and trigger point elasticity was measured using SWE. In the combined group, trigger point injection therapy involved marking and cleansing, followed by a US-guided injection of 3 mL of 0.5% lidocaine and 0.5% normal saline. Subsequent analysis revealed statistically significant reductions in pain, functional disability, skin temperature, and stiffness in both the shockwave and combined groups. The combined group exhibited a more pronounced reduction in stiffness than the shockwave group at 4 weeks. No significant differences in electrical activity were observed between the groups. Additionally, the combined group displayed notable differences in pain and stiffness compared with those of the shockwave group during the 4-week period. Overall, this study suggests that combining extracorporeal radial shockwave therapy with trigger point injection of lidocaine is more effective in alleviating pain and reducing stiffness associated with upper trapezius MPS.
Insights from a recent review on various guided injection targets
In 2023, Ricci et al. [7] introduced diverse interventional strategies for addressing cervical MPS, focusing on interventions such as injection and/or DN of trigger points, interfascial plane blocks, and fascial hydrodissection. For trigger points, accurate localization using US examination is crucial for prompt decision-making and precise targeting to avoid collateral damage. Employing a linear, high-frequency transducer and an in-plane technique enhanced the visualization during the procedure. The authors advocated a multistep injection process to effectively target the nociceptors. Emphasis was placed on the synergistic effects of combining DN with anesthetic injection to enhance the overall efficacy of MPS treatment (Fig. 5A).
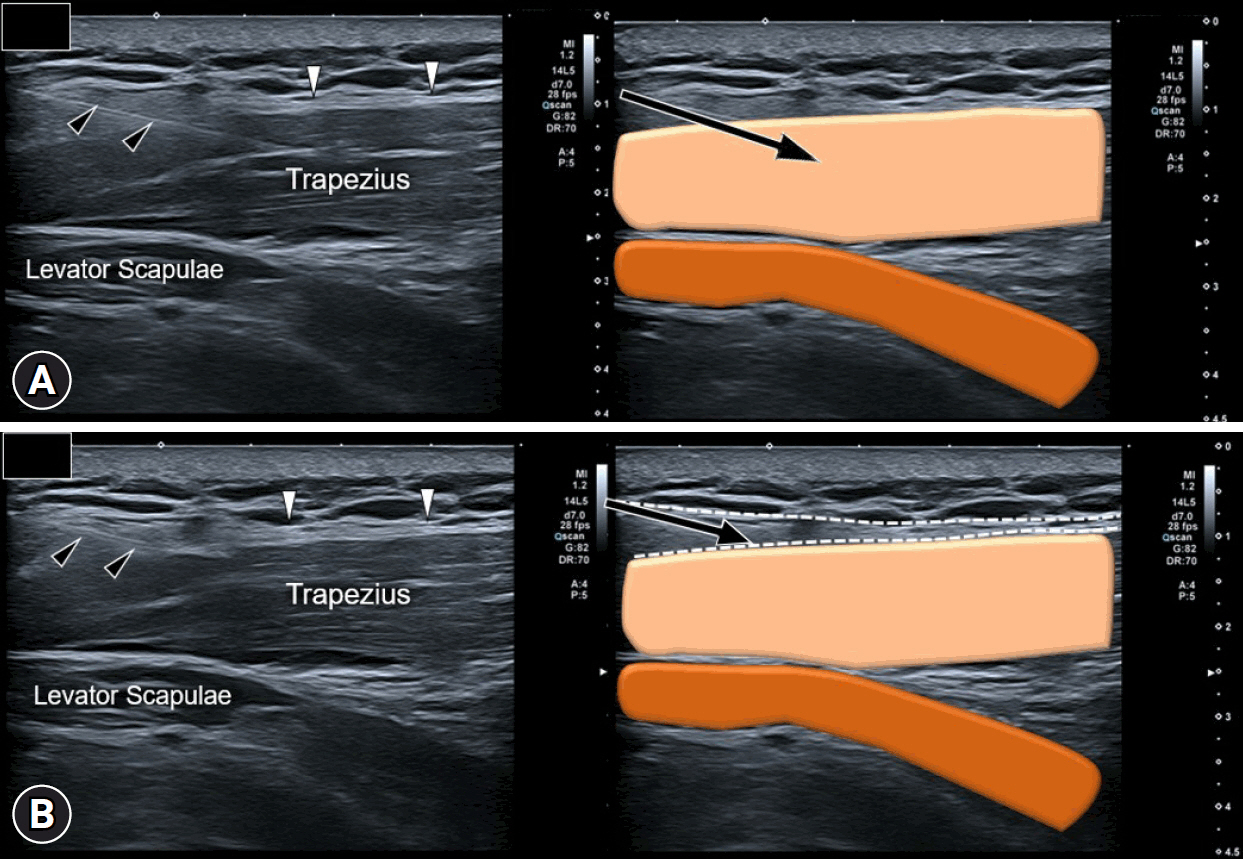
Ultrasound imaging (left side) and schematic drawing (right side) of ultrasound-guided procedures: (A) myofascial trigger point injection and (B) fascial hydrodissection. The black arrowheads point to the needle trajectory, while the white arrowheads indicate the superficial fascia in the subcutaneous tissue. The arrows represent the needle trajectory, whereas the dash lines indicate the fascia.
Interfascial plane blocks are recommended for individuals who experience diffuse cervical muscle contractions without detectable trigger points (Fig. 2). US-guided injections into interfascial planes aim to selectively block specific peripheral nerves, such as the supraclavicular and dorsal scapular nerves [13]. High-volume injections are recommended for efficient hydrodissection, particularly in patients with fibrosis. Safety considerations involve assessment of the surrounding vascular structures using power Doppler.
Fascial hydrodissection is an advanced interventional technique that targets the deep fascia, a highly innervated structure interconnected with the spinal nerves. This procedure entails a layer-by-layer high-volume injection to address intrafascial gliding and release adhesions (Fig. 5B). Technical recommendations include the use of a long and flexible needle for navigating through multiple fascial layers and employing a seeding technique for optimal mixture release.
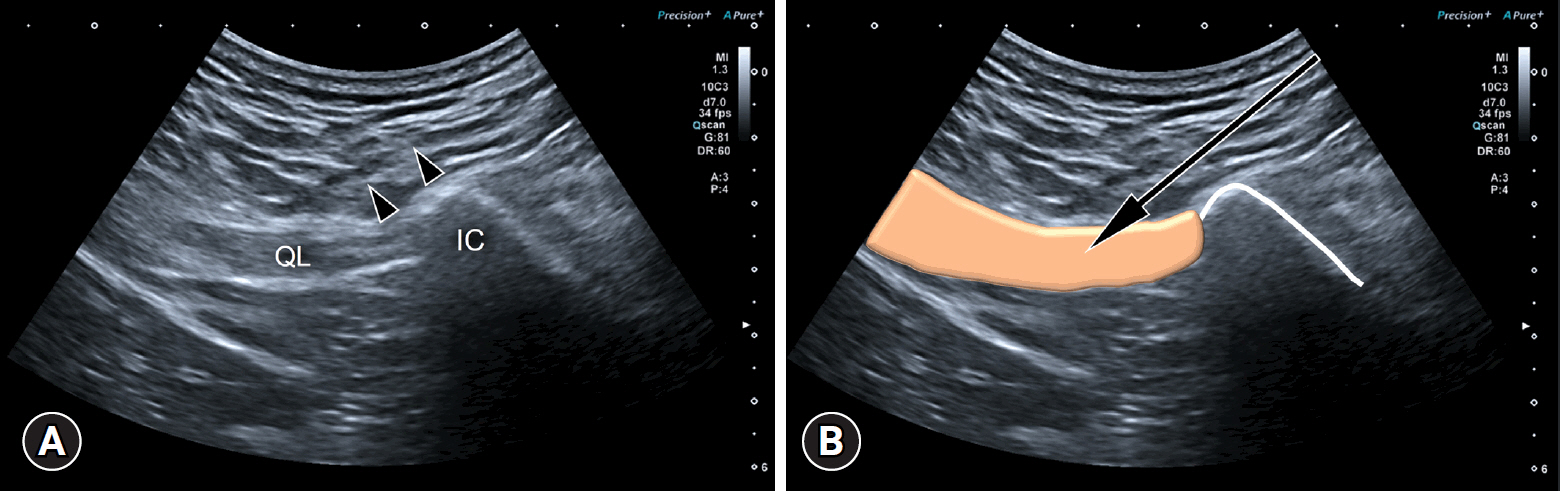
Ultrasonography-guided delivery of local anesthetics and steroids for quadratus lumborum myofascial pain syndrome
In 2023, Barreto Silva et al. [14] conducted a study to evaluate the efficacy of US-guided delivery of levobupivacaine and triamcinolone for quadratus lumborum MPS. This observational and retrospective study involved participants who underwent US-guided injection specifically targeting the quadratus lumborum muscles. Employing a low-frequency curvilinear probe positioned parallel to the iliac crest, along the midaxillary line, and oriented posteriorly to target the lateral interfascial triangle, a 22-gauge needle was directed in the lateral-medial and posterior-anterior directions. The region between the erector spinae muscle and posterior surface of the quadratus lumborum muscle was targeted (Fig. 6). Pain intensity was assessed using the 5-point NRS preintervention and 72 hours, 1 month, 3 months, and 6 months after intervention. The study included 90 participants with a mean age of 55.2 years, 68% of whom were females. A comparative analysis revealed improvements in pain lasting up to 3 months and sustained until 6 months after intervention. US-guided injection of the quadratus lumborum muscle was deemed a safe and effective procedure for managing pain in quadratus lumborum MPS within 6 months after intervention.
Conclusion
Different US examination techniques, including grayscale imaging and sonoelastography, can be utilized to assess changes in the echotexture and mechanical properties of the muscles affected by MPS. US guidance enhances the accuracy of needle placement in muscles affected by MPS, allowing targeted treatment. A range of US-guided interventions can be used to manage MPS, including IH, nerve hydrodissection, and intramuscular trigger point injections. To effectively address MPS, physicians can apply these techniques individually or in combination with other therapeutic modalities such as shockwave therapy.
Notes
Conflicts of interest
Wei-Ting Wu and Ke-Vin Chang have been editorial board members of Journal of Yeungnam Medical Science since 2021. They were not involved in the review process of this manuscript. There are no other conflicts of interest to declare.
Funding
This study was funded by the National Taiwan University Hospital, Bei-Hu Branch; Ministry of Science and Technology, Taiwan (MOST 106-2314-B-002-180-MY3 and MOST 109-2314-B-002-114-MY3) and National Science and Technology, Taiwan (NSTC 112-2314-B-002-134).
Author contributions
Conceptualization: all authors; Data curation, Investigation, Software: WTW, KVC; Formal analysis, Supervision: WTW, KVC, LÖ; Funding acquisition, Validation: WTW, KVC, VR; Project administration: WTW, LÖ; Visualization: WTW; Writing-original draft: WTW, KVC; Writing-review & editing: KVC, VR, LÖ.