Multilocular cystic hemangioma of the liver mimicking mucinous cystic neoplasm: a case report
Article information
Abstract
Hepatic hemangiomas infrequently exhibit atypical imaging features, which may cause diagnostic confusion with hepatic malignancies and lead to unnecessary surgery. We report a rare case of multilocular cystic hemangioma of the liver mimicking a mucinous cystic neoplasm of the liver in a 48-year-old female, focusing on computed tomography and magnetic resonance imaging features and their differential diagnosis.
Introduction
Cavernous hemangiomas are the most common benign tumors of the liver [1,2]. Mostly, imaging studies are sufficient for a definite diagnosis of typical cavernous hemangioma, and this lesion does not require surgical resection [1,2]. Infrequently, cavernous hemangiomas showing atypical imaging features are confused with other malignant hepatic tumors, which will subsequently require unnecessary surgery [3,4]. Cavernous hemangiomas containing fluid and multiple septa are rare. To our knowledge, there have been a few case reports on the imaging features of a multilocular cystic hemangioma of the liver [5-8]. In our case report, we present atypical imaging features of a multilocular cystic cavernous hemangioma with pathologic correlation.
Case
Ethical statements: This retrospective study was approved by the Institutional Review Board (IRB) of Pusan National University Hospital (IRB No: 2012-012-097), and the requirement for informed consent from the patient was waived by the IRB.
A 48-year-old female presented with lower abdominal pain and menorrhagia, and multiple uterine myomas were detected during a transvaginal ultrasound examination. She underwent contrast-enhanced abdominal computed tomography (CT) in the obstetrics and gynecology department for a preoperative examination of uterine myomas. On a CT scan, a hepatic tumor was incidentally found. CT scan revealed an approximately 14-cm multiseptated cystic mass containing some enhancing irregular septa in the right lobe of the liver (Fig. 1). For a detailed investigation of the hepatic tumor, gadoxetic acid-enhanced magnetic resonance imaging (MRI) of the liver was performed, which also revealed a huge multiseptated cystic mass with T1-hypointensity and T2-hyperintensity, identical to that of the fluid. Some hemorrhagic locules showing T1-hyperintensity and T2-hypointensity were noted (Fig. 2A, 2B). Enhancement of the irregular septa within the tumor was observed, but no solid enhancing nodules were detected (Fig. 2C). She did not complain of any symptoms related to the hepatic tumor. Laboratory tests, including liver function tests and tumor markers such as cancer antigen (CA) 125, carcinoembryonic antigen, alpha-fetoprotein, and CA 19-9 were unremarkable. No metastasis was found on the chest or abdominal CT.

Computed tomography (CT) findings of a multilocular cystic hemangioma of the liver in a 48-year-old female. Contrast-enhanced dynamic-phase abdominal CT scans show a huge septated cystic mass in the right lobe of the liver. (A) Nonenhanced, (B) arterial phase, (C) portal venous phase, and (D) delayed phase. Enhancement of the septa within the mass (arrows) is noted.
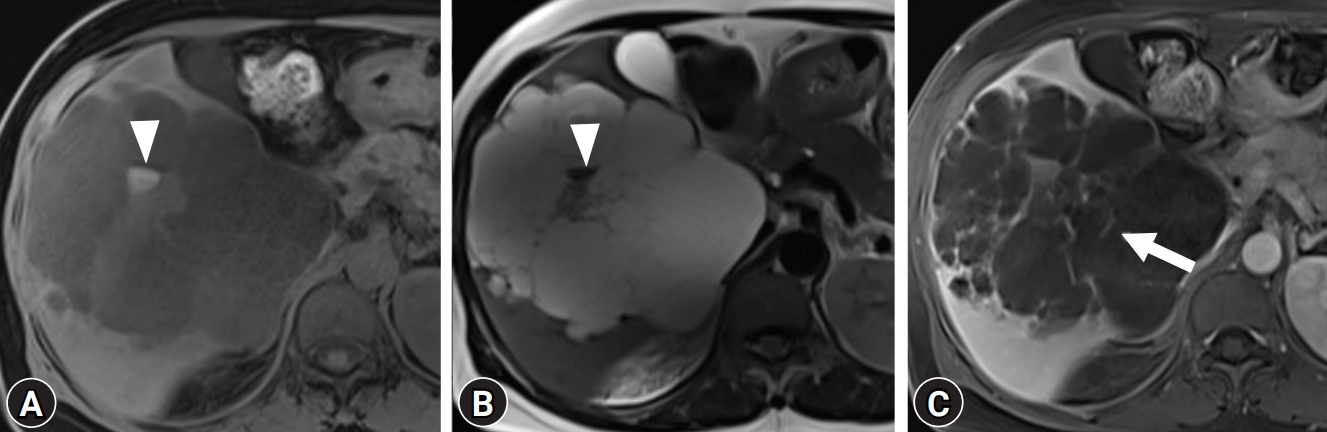
Magnetic resonance imaging findings of a multilocular cystic hemangioma of the liver in a 48-year-old female. (A) T1-weighted and (B) T2-weighted images show a multiseptated cystic mass containing variable signal intensity. Most locules present as T1-hypointensity and T2-hyperintensity, identical to signal intensity of fluid. Some T1 hyperintense locules present as T2-hypointensity, suggesting subacute hemorrhage (arrowheads). (C) Contrast-enhanced fat-suppressed T1-weighted image shows septal enhancement (arrow).
Based on these imaging features, we considered the possibility of a mucinous cystic neoplasm (MCN) of the liver. Under high suspicion of hepatic MCN and consideration of large tumor size, the surgeon decided to perform immediate surgery without cytologic aspiration or biopsy. Bisectionectomy of the liver (resection of Couinaud segments 5 and 6) was performed. Histological examination of the resected tumor specimen revealed a well-defined multiseptated cystic mass in the liver, containing fluid, necrosis, and hemorrhage (Fig. 3A). Microscopic findings showed a multilocular cystic mass composed of variable-sized cystic spaces (Fig. 3B) and a cystic wall lined by flattened or cuboidal endothelial cells without cytologic atypia and supported by stroma (Fig. 3C). On immunohistochemical staining, the endothelial cells were positive for vascular endothelial cell markers (ETS-related gene [ERG], CD34, and factor VIII), but negative for biliary epithelial cell markers (cytokeratin 7 [CK 7] and CK 19) (Fig. 3D–F). The final diagnosis was a multilocular cystic cavernous hemangioma.

Histopathologic findings of a multilocular cystic hemangioma of the liver in a 48-year-old female. (A) The cut section of the gross specimen shows multiple cystic loculi separated by multiple septa. (B) Low-power magnification shows a multilocular cystic mass composed of medium to small-sized cystic space (hematoxylin and eosin [H&E] stain, ×40). (C) High-power magnification shows the cystic wall lined by flattened or cuboidal endothelial cells without cytologic atypia and supported by fibrotic stroma (H&E stain, ×200). On immunohistochemical staining, the endothelial cells are positive for vascular endothelial cell markers such as (D) ETS-related gene (ERG), (E) CD34, and (F) factor VIII (immunohistochemical stain, ×200 [D-F]), but negative for biliary epithelial cell markers such as cytokeratin 7 (CK 7) and CK 19 (not shown).
Discussion
Vilgrain et al. [3] described less frequent atypical imaging patterns of liver hemangiomas, such as large heterogeneous giant hemangiomas, rapidly filling hemangiomas, calcified hemangiomas, hyalinized hemangiomas, cystic or multilocular hemangiomas, hemangiomas with fluid-fluid levels, and pedunculated hemangiomas. According to Vilgrain et al. [3], our case may be categorized as cystic or multilocular hemangioma.
To our knowledge, only four cases of multilocular cystic hemangioma of the liver along with their CT and/or MRI findings, have been reported previously [5-8]. The size of the mass in the previous cases was approximately between 3.5 cm and 6 cm. The common imaging features were a well-defined multilocular cystic lesion showing hypoattenuation on CT and bright hyperintensity on T2-weighted MRI. It also showed a lobulated margin and some irregular septa. Three reports described the enhancing portion of the tumor, and among these, Cha et al. [8] performed dynamic-phase contrast-enhanced CT, which did not show globular enhancement seen in typical hemangiomas, but delayed gradual enhancement was noted in the central portion [5,6,8]. Another case did not show any enhancement on contrast-enhanced imaging [7]. Similar to previous cases, our case also showed a multilocular cystic lesion with bright T2 hyperintensity, lobulated margins, and some irregular septa. However, the mass in our case was larger (about 14 cm) than those in previously reported cases, and there was no enhancing portion except for the septa.
Multilocular cystic hepatic lesions are commonly detected on CT and MRI; however, they are nonspecific and cause potential challenges for differential diagnosis [9,10]. MCN is a rare neoplasm of the liver. Complete resection is required because of its malignant potential. The MCN of the liver appears as a large, solitary, multilocular cystic lesion with well-circumscribed margins and internal septa. Enhancement is commonly observed along the walls and internal septa. Some enhancing solid portions may exist in mucinous cystadenocarcinomas. It has been reported exclusively in middle-aged female patients with ovarian-like stroma within the tumor [9,10]. Hepatocellular carcinoma (HCC) may lead to extensive necrosis or hemorrhage, which can manifest as an atypical multilocular cystic mass. Noticeably, even multilocular cystic HCC demonstrates mural nodules with arterial enhancement and delayed washout pattern or delayed capsular enhancement, which is indicative of typical HCC. Moreover, a hepatic mass in cirrhosis should first be considered HCC [9,10]. Multilocular cystic metastasis can be caused by extensive necrosis of hepatic metastasis, especially from a neuroendocrine tumor, melanoma, or gastrointestinal stromal tumor, or abundant mucin production from mucinous adenocarcinoma of the ovary or colorectum. Enhancing irregular septa or walls may present viable tumor cells within the cystic metastasis. However, because these imaging findings are usually nonspecific compared with other multilocular cystic neoplasms, knowledge of their primary malignancy is the most important [9,10]. Non-neoplastic hepatic lesions include hepatic abscesses, echinococcal cysts, intrahepatic hematomas, and bilomas. Hepatic abscesses generally show characteristic imaging features, such as the cluster sign or double target sign, and are associated with febrile conditions. A typical echinococcal cyst appears as a mother cyst and peripheral daughter cysts, which are associated with endemic areas. Intrahepatic hematoma or biloma may be associated with trauma or iatrogenic injuries [9,10]. Therefore, in our case, considering the past history of no primary malignancy, trauma, or travel, and that the patient was asymptomatic and a middle-aged female, MCN of the liver was the most likely preoperative diagnosis.
The pathogenesis of hemangioma multilocularity remains unknown. According to previous literature, it may be caused by cystic degeneration secondary to thrombus formation, necrosis or hemorrhage, and scar formation within cavernous hemangioma [6,7]. Similar to previous reports, our imaging features are also correlated with macroscopic appearance, showing a multiseptated cystic lesion containing fluid, necrosis, and hemorrhage. In our case, septa showed delayed enhancement that might be a fibrous stroma rather than centripetal filling-in enhancement in typical hemangioma [8].
Multilocular cystic hemangiomas are extremely rare and difficult to differentiate from other cystic hepatic lesions. Therefore, it is important to be familiar with the fact that hemangiomas can rarely be seen as multilocular cystic hepatic lesions. If other differential diagnoses in multilocular cystic hepatic lesions are excluded, the possibility of atypical hemangioma is suspected, and preoperative biopsy can be performed to avoid unnecessary extended hepatic resection.
Notes
Conflicts of interest
No potential conflicts of interest relevant to this article were reported.
Funding
This work was supported by clinical research grant from Pusan National University Hospital in 2020.
Author contributions
Conceptualization, Project administration: SK, NKL; Data curation, Formal analysis: SBH, SJL, HIS; Funding acquisition: NKL; Writing-original draft: NKL; Writing-review & editing: SK, NKL.
