Intensive care unit management of uncomplicated type B aortic dissection in relation to treatment period: a retrospective observational study
Article information
Abstract
Background
Medical therapy is the standard treatment for uncomplicated acute type B aortic dissection (ATBAD), but there is little evidence of the need for intensive care unit (ICU) management. Therefore, we aimed to investigate the effects of ICU treatment on uncomplicated ATBAD.
Methods
We retrospectively studied patients with uncomplicated ATBAD who were medically treated between January 2010 and July 2020. Patients were divided into short-term ICU stay (SIS) and long-term ICU stay (LIS) groups, according to a 48-hour cutoff of ICU stay duration. The incidence of pneumonia and delirium, rate of aortic events, hospital mortality, and survival rate were compared.
Results
Fifty-five patients were treated for uncomplicated ATBAD (n=29 for SIS and n=26 for LIS). The incidence of pneumonia (3.6% vs. 7.7%) and delirium (14.3% vs. 34.6%) was higher in the LIS group than in the SIS group, but the differences were not statistically significant. The survival rates at 1, 3, and 5 years were not different between the two groups (SIS: 96.4%, 92.2%, and 75.5% vs. LIS: 96.2%, 88.0%, and 54.2%, respectively; p=0.102). Multivariate Cox regression analysis for aortic events showed that using a calcium channel blocker lowered the risk of aortic events.
Conclusion
Long-term ICU treatment is unlikely to be necessary for the treatment of uncomplicated ATBAD. Active use of antihypertensive agents, such as calcium channel blockers, may be needed during the follow-up period.
Introduction
Type B aortic dissection remains a challenging disease to treat, with high morbidity and mortality despite advances in therapeutic techniques. Although endovascular treatment of type B aortic dissection has increased based on the INSTEAD (the INvestigation of STEnt Grafts in Aortic Dissection) and INSTEAD-XL (INSTEAD with extended length of follow-up) trials, it remains a class IIa recommendation for uncomplicated type B aortic dissection [1-3]. Optimal medical therapy is a class I recommendation and plays an important role in the treatment of uncomplicated acute type B aortic dissection (ATBAD). In the current academic world, studies on the effectiveness of endovascular therapy are prevalent, but there is little interest in determining optimal medical therapy and its effect on long-term results. In the initial treatment of ATBAD, most medical centers incorporate intensive care unit (ICU) treatment, but the need for ICU-level care is different for each patient, and the long-term results associated with the need for ICU treatment are not well known. ICU treatment is clearly a necessity in the management of ATBAD, but it may lead to pneumonia or mental stress in some patients. If these complications occur in patients with ATBAD, they may be harmful during the course of initial optimal medical therapy, which may have a negative effect on the patient’s subsequent clinical course. In addition, there are no well-documented factors that affect the long-term course and survival rate of uncomplicated ATBAD. Therefore, we investigated the clinical course of patients with uncomplicated ATBAD, focusing on the impact of ICU treatment and medical management, as well as the effects of antihypertensive medication use on long-term outcomes after discharge.
Methods
Ethical statements: This study was approved by the Institutional Review Board (IRB) of Daegu Catholic University Medical Center (IRB No: CR-18-138-L). Patient consent was waived owing to the retrospective nature of the study.
1. Study population and data collection
Between January 2010 and July 2020, 85 patients treated with ATBAD at Daegu Catholic University Medical Center were enrolled in this study. ATBAD was defined as a new dissecting or intramural hematoma lesion confined only to the descending aorta and identified on radiologic images within 2 weeks of symptom onset. Patients treated for complicated type B aortic dissection were excluded from this study. Data were collected retrospectively, and medical records and diagnostic imaging data were used. Patients whose mortality was unclear were considered to have died when they lost their health insurance. We investigated sex, age, and past medical history as the baseline characteristics. The duration of ICU stay, overall hospital stay, incidence of complications including 30-day mortality, and medications prescribed after discharge were also investigated. Follow-up data were obtained for survival rate and aortic event-free survival. Aortic events were defined as those that required surgical intervention during the follow-up period. The patients were divided into a long-term ICU stay (LIS) group and a short-term ICU stay (SIS) group, based on an ICU hospitalization cutoff of 48 hours.
The primary endpoints were death and aortic events. The survival rate and aortic event-free survival rate of the two groups were compared. Risk factors associated with survival were also investigated. The secondary endpoints were pneumonia and delirium during admission.
2. General principle of acute type B aortic dissection management
Patients with ATBAD at our center were initially admitted to the ICU. Although the basic strategy was an ICU stay of 1 week, sometimes, there was insufficient capacity in the ICU; thus, in some cases, patients were admitted to the general ward or were discharged from the ICU earlier than scheduled. All patients received a central and arterial line with real-time blood pressure monitoring. Urine volume was measured hourly via a bladder catheter, and patients were maintained nil per os until their condition stabilized. A calcium channel blocker or β-blocker was infused intravenously. During hospitalization, all patients were managed to maintain a systolic blood pressure of less than 120 mmHg, were prescribed restricted ambulation, and were administered a bowel softener. When the patient’s blood pressure or symptoms stabilized, the intravenous antihypertensive medication was switched to an oral formulation. If the patient was initially admitted to the general ward, the central line was used for administration of the intravenous antihypertensive medication, and blood pressure was measured manually every hour. When the patient’s blood pressure and symptoms stabilized, the antihypertensive medication was switched to an oral formulation. Other management concerns were the same in both of these groups. Follow-up computed tomography (CT) was performed 1 week and 2 weeks after admission. If the CT images at 1 week were favorable, ambulation was allowed if the patient had been discharged from the ICU. When there was no progression of aortic dissection on the CT images at 2 weeks, discharge on oral antihypertensive medications was considered. If there were findings of ongoing dissection, such as intractable pain, bowel ischemia, rapid expansion of the aortic aneurysm, or uncontrolled blood pressure, surgical intervention was planned. After discharge, the patients were followed up for 3 to 6 months in an outpatient clinic with annual CT imaging.
3. Statistical analysis
Categorical data are expressed as frequencies and percentages, and continuous data are expressed as mean±standard deviations with ranges. The chi-square test or Fisher exact test was used for categorical data, and the Mann-Whitney test was used for continuous data. The Kaplan-Meier method was used to obtain survival rates and freedom from aortic events. Survival rates were compared using the log-rank test. For the multivariate analysis, Cox proportional hazard models were used to investigate risk covariates affecting the endpoints of both groups. Multivariate analysis was performed on univariate analysis covariates with p-values of <0.3. The results are expressed as hazard ratios with 95% confidence intervals, and p<0.05 was considered statistically significant. All statistical analyses were performed using IBM SPSS ver. 25 (IBM Corp., Armonk, NY, USA).
Results
1. Study population
Eighty-five patients were treated for ATBAD during the study period. Of these, 55 consecutive patients with uncomplicated ATBAD were included in the study; 27 patients who underwent surgical treatment for complicated ATBAD and three patients who were denied treatment or referred to other hospitals were excluded. The reason for surgical treatment was complicated ATBAD in nine patients and traumatic lesions in 18 patients. Among the 27 patients who underwent surgical treatment, stent-graft implantation was performed in all of them, with the exception of one patient in whom vascular access was difficult. All patients with trauma underwent emergency surgery. The mean duration from the diagnosis of uncomplicated to complicated ATBAD was 3.67±1.33 days, and all patients showed worsening clinical status during ICU management. Of the 55 patients, 29 stayed in the ICU for less than 48 hours.
2. Baseline characteristics
Table 1 summarizes the baseline characteristics of the patients. The mean patient age was 65.38±14.25 years and 43.6% were female. The mean duration of ICU stay and mean duration of total hospital stay were 3.51±4.40 days and 17.96±8.25 days, respectively. There was no difference in demographic characteristics between the two groups.
3. Early outcomes
There was one case of 30-day mortality in the LIS group. The cause of death was pneumonia complicated by sepsis. The incidence of pneumonia in the SIS and LIS groups during the hospitalization period was 1 of 29 (3.4%) and 2 of 26 (7.7%), respectively. The incidence of delirium in the SIS and LIS groups was 4 of 29 (13.8%) and 9 of 26 (34.6%), respectively. There was no statistically significant difference between the two groups in terms of pneumonia and delirium, but the incidence of delirium was higher in the LIS group (p=0.07). The mean duration from admission to the onset of pneumonia and delirium was 4.33±4.03 days and 4.31±1.86 days in the SIS and LIS groups, respectively.
4. Late outcomes
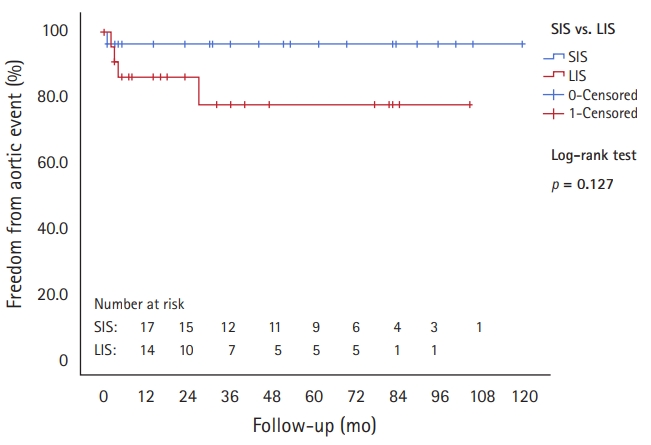
The mean follow-up period was 58.51±37.85 months (range, 1–127 months) without an intergroup difference (p=0.26). There were 17 deaths during the follow-up period, of which 10 were in the LIS group. The overall survival rates at 1, 3, and 5 years were 96.6%, 79.8%, and 75.6% in the SIS group and 96.2%, 77.9%, and 54.2% in the LIS group, respectively (Fig. 1). There was no difference in survival rate between the groups (p=0.102). The rate of survival without aortic events requiring surgical intervention at 5 years was 96.3% in the SIS group and 77.5% in the LIS group (Fig. 2); this difference was not statistically significant (p=0.127). A post hoc power analysis was performed using two types of events, death and aortic events, resulting in a power of 0.802 and 0.816, respectively.

Kaplan-Meier curves for survival in the short-term intensive care unit stay (SIS) and long-term intensive care unit stay (LIS) groups.
5. Antihypertensive medications
All patients except two were prescribed antihypertensive medication after discharge, including at least one β-blocker, calcium channel blocker, angiotensin-related antihypertensive (ARA), or diuretic (Table 2). The prescription rates for β-blockers, calcium channel blockers, ARAs, and diuretics were 76.4%, 67.3%, 30.9%, and 38.2%, respectively. Two patients received only one type of antihypertensive medication, while all others received combination therapy. There was no difference in the prescription of antihypertensive medications between the two groups.
6. Risk factors affecting survival and aortic events
Risk factors were investigated using several variables to determine factors affecting long-term survival. In the univariate analysis, covariates including female sex, current smoking status, history of chronic obstructive pulmonary disease, calcium channel blocker use, and ARA use correlated with survival. However, in the multivariate analysis of survival and these covariates, there was no significant correlation (Table 3). In the univariate analysis of aortic events, four covariates, female sex, history of hypertension, calcium channel blocker use, and LIS, correlated. Unlike the results for survival, multivariate analysis showed a statistically significant association between aortic events and history of hypertension and calcium channel blocker use (Table 3).
Discussion
Management of patients with ATBAD in the ICU, particularly patients who are elderly, increases the risk of mental stress, which can lead to delirium [4]. When delirium occurs, it makes pulmonary care challenging, with an increased risk of pneumonia, and increases the difficulty in managing blood pressure or aortic symptoms [5,6]. This study initially aimed to investigate whether ICU treatment of uncomplicated ATBAD is necessary. The ICU environment is inevitably stressful for patients. Can these patients be treated adequately in the general ward with less mental stress, simply by frequently monitoring blood pressure and evaluating changes in symptoms? With the many limitations of our study, we cannot provide a complete answer to this question. However, there was a pioneering study with a context similar to ours. Niino et al. [7] showed that patients in an early ambulation group via an optimal clinical pathway had reduced respiratory complications and delirium, but these investigators found no differences in terms of early mortality and change in aortic size 1 month after symptom onset when compared to patients with long-term bed rest in the ICU. As mentioned earlier, recent interest in academia has focused on endovascular treatment. However, the importance of optimal medical therapy is still fundamental, and if medical therapy is not appropriately optimized, it will be necessary to actively improve our understanding via research. We are not advocating medical treatment only for uncomplicated ATBAD. The importance of endovascular treatment in the management of uncomplicated ATBAD is well recognized, and there is no intent to challenge this fact.
A cutoff value was needed to divide the groups based on the duration of ICU admission, but the most appropriate value could not be obtained from our data because the number of included patients was too small. The distribution of the two groups based on defining a prolonged ICU stay of 48 hours or longer was based on previous studies [8-11]. As reported by Ely et al. [4], delirium occurs initially in the ICU between the second and third days. In addition, one of our study aims was to address whether long-term ICU treatment was associated with increased delirium. Among the nine patients with delirium in the LIS group, two patients developed delirium within 48 hours and seven patients developed delirium after 48 hours.
The use of β-blockers in chronic type B aortic dissection is known to reduce the progression of aortic dilatation, incidence of subsequent hospital admissions, incidence of late dissection-related aortic procedures, and cost of treatment [12-17]. Our policy for prescribing antihypertensive medications was to use a β-blocker as the first choice of drug, unless bradycardia was identified, in which ARA or calcium channel blockers were more appropriate. Jonker et al. [18] reported that the use of calcium channel blockers reduced aortic expansion after ATBAD. Our results also showed that the use of calcium channel blockers reduced the aortic event rate during the follow-up period. Considering the tendency to control blood pressure using a calcium channel blocker in patients who are active outpatients and are sensitive to blood pressure control, strict blood pressure control may be important during the follow-up period.
In the initial treatment of ATBAD, ICU treatment is not essential if the patient’s blood pressure and symptom progression can be monitored. Rather, ICU treatment exacerbates patient mental stress, increasing the risk of delirium, but does not seem to affect long-term survival or aortic events. However, ATBAD still has a poor long-term survival rate and an increased risk of aortic complications. The active use of antihypertensive agents, such as calcium channel blockers, may be needed during the follow-up period.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Funding
This work was supported by the grant of Research Institute of Medical Science, Catholic University of Daegu (No. 202015).
Author contributions
Conceptualization, Data curation, Formal analysis, Methodology: all authors; Funding acquisition, Validation: JWC, JSJ; Investigation: CHL; Supervision: JWC; Writing-original draft: CHL, JSJ; Writing-review & editing: JWC.