PubMed Central, CAS, DOAJ, KCI

Articles
- Page Path
- HOME > J Yeungnam Med Sci > Volume 40(1); 2023 > Article
-
Case report
Scrotal pyocele secondary to gastrointestinal perforation in infants: a case series -
Soo-Hong Kim1,2
 , Yong-Hoon Cho1,2
, Yong-Hoon Cho1,2 , Hae-Young Kim2
, Hae-Young Kim2 , Narae Lee3
, Narae Lee3 , Young Mi Han3
, Young Mi Han3 , Shin Yun Byun3
, Shin Yun Byun3
-
Journal of Yeungnam Medical Science 2023;40(1):86-90.
DOI: https://doi.org/10.12701/yujm.2021.01508
Published online: December 15, 2021
1Division of Pediatric Surgery, Department of Surgery, Pusan National University Yangsan Hospital and Pusan National University Children’s Hospital, Yangsan, Korea
2Division of Pediatric Surgery, Department of Surgery, Pusan National University School of Medicine, Busan, Korea
3Division of Neonatology, Department of Pediatrics, Pusan National University Children’s Hospital, Yangsan, Korea
- Corresponding author: Yong-Hoon Cho, MD Division of Pediatric Surgery, Department of Surgery, Pusan National University Yangsan Hospital, 20 Geumo-ro, Mulgeum-eup, Yangsan 50612, Korea Tel: +82-55-360-2124 Fax: +82-55-360-2154 E-mail: choyh70@pusan.ac.kr
Copyright © 2023 Yeungnam University College of Medicine, Yeungnam University Institute of Medical Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
- Pyocele in infants is rarely described in the literature, but it is an emergent condition that requires rapid recognition and treatment to prevent testicular loss. If peritonitis due to gastrointestinal perforation occurs, abdominal contamination may spread through a patent processus vaginalis in an infant, which may lead to pyocele. We report the cases of three infants with scrotal pyocele due to the spread of infection or inflammatory material from the intraperitoneal cavity through a patent processus vaginalis. Two infants were surgically treated, while the other was treated with percutaneous aspiration and intravenous antibiotic administration. Although rare, pyocele should be considered in the differential diagnosis of acute scrotum in infants, especially in infants who previously had peritonitis due to gastrointestinal perforation.
- Scrotal swelling is common among neonates and infants; however, its etiology varies. Most of these diseases, such as hydroceles, do not require prompt treatment [1]. One rare cause of scrotal swelling is scrotal pyocele, which is also very rare in neonates and infants. Scrotal pyocele should be treated immediately, and when treatments fail, orchiectomy may be required [2].
- There are various etiologies of scrotal pyocele in infants. In patients with peritonitis due to gastrointestinal perforation, the spread of infection or inflammatory material from the intraperitoneal cavity through a patent processus vaginalis could be causative [3]. Herein, we report three cases of scrotal pyocele related to peritonitis due to gastrointestinal perforation in neonates and present a brief literature review.
Introduction
- The patients’ characteristics are summarized in Table 1.
- 1. Case 1
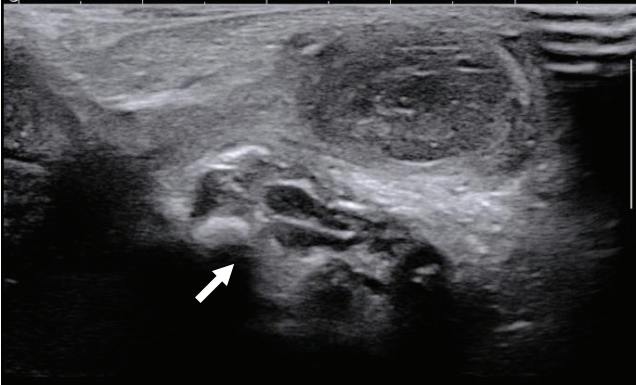
- A 5-day-old male neonate was transferred to our neonatal intensive care unit due to necrotizing enterocolitis. He was born at 38 weeks and 5 days of gestation via normal vaginal delivery, weighing 3,360 g. Before the transfer, his oral intake was poor, he was vomiting bile-colored contents, and his abdomen was distended. An emergent exploratory laparotomy was performed after an infantogram revealed pneumoperitoneum. A gastric perforation from the fundus to the mid-body along the lesser curvature was observed, and primary closure was performed. Right scrotal swelling and fever (up to 37.4°C) were noted 4 days after the surgery. Serum C-reactive protein (CRP) level was high at 5.08 mg/dL (range, <0.5 mg/dL); other laboratory findings were within normal limits. Ultrasonography revealed complex fluid collection in the right scrotum, accompanied by multiple amorphous calcifications (Fig. 1). Vascular flow between the right testis and spermatic cord was preserved. With an inguinal incision, high ligation of the patent processus vaginalis, and irrigation and drainage of the abscess were performed. Intravenous cefotaxime was injected. Because the swelling and redness of the scrotum persisted, we recognized a remnant abscess. Thus, 2 weeks later, we performed an additional scrotal incision and drainage due to the remnant abscess. After the second operation, intravenous cefotaxime was administered for 2 more weeks. Three weeks after the second incision and drainage, the patient was discharged without any other problems. Follow-up ultrasound examination after 6 months revealed no abnormal findings in the testes and scrotum.
- 2. Case 2
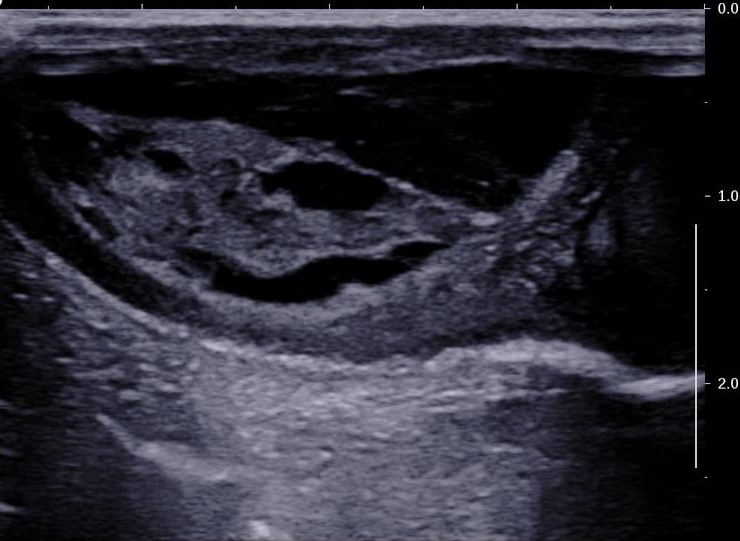
- A male neonate, born at 37 weeks and 1 day of gestation via normal vaginal delivery, weighing 3,290 g, was referred due to abdominal distension and scrotal swelling (Fig. 2). On prenatal ultrasonography, fetal ascites was found, and fetal bowel perforation was suspected. The next day, an explorative laparotomy was performed. Operative findings revealed ileal atresia and generalized peritonitis due to small bowel perforation. Small bowel segmental resection and anastomosis were performed. After the surgery, feeding intolerance did not improve and the scrotum, which collapsed immediately after surgery, gradually swelled the next day, leading to redness and a heating sensation. Vital signs, whole blood cell counts, and serum CRP levels were within normal limits. An upper gastrointestinal series and colon studies showed delayed contrast passage in the small bowel. Because passage disturbance at the anastomosis site or intestinal motility disorder was considered based on the contrast studies, loop ileostomy was planned. Ultrasonography revealed a complex right scrotal hydrocele with a patent processus vaginalis (Fig. 3). Scrotal exploration was performed with loop ileostomy. The patent processus vaginalis was closed on the peritoneal side. The complex fluid was removed using a scrotal incision, and a drainage tube was inserted. Methicillin-resistant Staphylococcus epidermidis and Enterococcus faecium were cultured from a pyocele. Intravenous vancomycin was administered. Two days after the surgery, the drainage tube was removed, and the pyocele had healed. Six months later, the patient underwent ileostomy repair and was discharged. He is scheduled to undergo surgery for a buried penis when he is 2 years old.
- 3. Case 3
- A 7-day-old boy presented with abdominal distension. He was born by cesarean section due to premature rupture of the membranes at 27 weeks and 5 days of gestation, weighing 1,151 g. After birth, respiratory distress syndrome and persistent pulmonary hypertension were diagnosed, and surfactant and nitrogen oxides were administered and tapered. After transfer, pneumoperitoneum was found on an infantogram; thus, an exploratory laparotomy was performed immediately. A perforation site in the stomach along the greater curvature from the gastroesophageal junction to the mid-body was found, and the perforation was repaired. Two weeks after the surgery, desaturation occurred. Serum CRP level was elevated to 4.11 mg/dL and Escherichia coli was cultured from the peripheral blood. Physical examination revealed left inguinal swelling. Ultrasonography revealed bilateral small patent processus vaginalis and a left inguinal abscess connected to the left patent processus vaginalis (Fig. 4). The abscess was aspirated (Fig. 5), and intravenous meropenem was administered. E. coli was also cultured from the abscesses. After 10 weeks, the patient was discharged without any complications, and an intact testis was confirmed on follow-up sonography.
Cases
- Pyocele is also known as an infected hydrocele and scrotal abscess [4,5]. To date, only approximately 30 cases have been reported in patients younger than 18 months of age, and few of these are neonatal cases [2,6].
- Pyocele has various etiologies, including hematogenous spread, secondary infection from neighboring structures such as the testis or epididymitis, and spread through a patent processus vaginalis [3]. Cases associated with maternal sepsis or idiopathic cases have also been reported [6]. In particular, the proportion of preterm cases (e.g., case 3 in this report) with a patent processus vaginalis, which is connected to the peritoneal cavity, is relatively high. With neonates or infants, especially premature infants who have undergone surgery for peritonitis due to gastrointestinal perforation, the incidence might be relatively high due to the presence of the processus vaginalis. Careful observation of scrotal swelling is necessary.
- Because patent processus vaginalis is prevalent in males, most cases of infantile pyocele are male patients. However, in girls, hydroceles could also develop through a patent processus vaginalis, also called the canal of Nuck [7]. A female infant with a pyocele in the inguinal area through a patent processus vaginalis has also been reported [8].
- The symptoms of pyocele are not significantly different from those of other disorders with scrotal swelling. Tense scrotal edema and overlying skin erythema are common symptoms [3]. In particular, this erythema was helpful in identifying pyocele rather than simple hydrocele in this study. The silk gloves sign, for a patent processus vaginalis, was difficult to interpret in all three cases in this study due to swelling of neighboring tissues.
- Doppler ultrasonography was accurate in diagnosing pyocele in patients with scrotal swelling [6]. Doppler ultrasonography is useful in differentiating other diseases that produce acute scrotum, such as testicular torsion, epididymitis, and orchitis [9]. Ultrasonography revealed fine multiple septations, a fluid-fluid level with a dependent area of increased echogenicity, thickening of the scrotal layers, and layering debris [1,3]. When pyocele is suspected, it is recommended to perform Doppler ultrasonography quickly for differential diagnosis and immediate treatment.
- Various organisms have been reported to cause pyoceles. The majority of reported cases of spreading through a patent processus vaginalis have revealed infection with E. coli, and other idiopathic cases have revealed the involvement of Staphylococcus aureus, S. epidermidis, enterococci, Citrobacter freundii, and Staphylococcus hominis [2,3]. Sometimes, the culture results would be negative due to the effects of immediate antibiotic administration [3,10].
- Surgical exploration and drainage with intravenous antibiotic administration are the most commonly used treatment options. Scrotal incisions are more commonly used than inguinal incisions [3,5,6,8,11]. When surgeries are performed, the patent processus vaginalis should be repaired, if possible, to prevent ascending infection into the peritoneum and potential inguinal hernia [11]. However, the tissue of the patent processus vaginalis could be very fragile due to infection and inflammation; therefore, repair could be very difficult [3]. Some studies have shown favorable outcomes with percutaneous aspiration of abscesses and intravenous antibiotic administration. This method has the advantage of avoiding general anesthesia and is applicable to patients in poor general health [2,3]. Because various microorganisms, including antibiotic-resistant bacteria, should be considered causative organisms, the administration of broad-spectrum antibiotics should be performed first, followed by antibiotic adjustment according to culture results, regardless of whether surgical drainage or aspiration is performed. Appropriate treatment options should be selected according to the severity of the disease or the condition of the patient.
- There are no clear criteria or recommendations for which cases require surgical drainage or aspiration only. In cases 1 and 2, the abscesses were organized and seemed to be difficult to aspirate. The abscesses were larger in cases 1 and 2 than in case 3. In case 3, the abscess was also in a liquefied state and nearly complete aspiration was performed. Therefore, in our experience, for large and organized abscesses, surgical drainage is preferred; in contrast, for small and liquefied abscesses, aspiration should be attempted first.
- There are few reports on the long-term condition of the testis after treatment; therefore, it is difficult to determine prognosis. In our experience, when properly treated, the testes are well preserved. However, there was a report of orchiectomy due to severe inflammation and the risk of overwhelming sepsis [5].
- In summary, when scrotal swelling is encountered in infants or neonates, pyoceles should be included in the list of differential diagnoses. Careful attention is needed for infants, especially preterm infants who previously had peritonitis due to gastrointestinal perforation. If a pyocele is suspected, Doppler ultrasonography should be performed quickly and appropriate treatment initiated so that favorable results can be obtained without losing the testis.
Discussion
-
Ethical statements
This study was approved by the Institutional Review Board (IRB) of Pusan National University Yangsan Hospital (IRB No: 05-5021-198), and the requirement for informed consent from the patients was waived by the IRB.
-
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
-
Funding
This work was supported by a clinical research grant from Pusan National University Yangsan Hospital in 2021.
-
Author contributions
Conceptualization: SHK, YHC; Data curation: NL, YMH, SYB; Formal analysis: SHK, HYK; Investigation: YHC; Funding acquisition: SHK; Writing-original draft: SHK; Writing-review & editing: YHC, HYK.
Notes

- 1. Basta AM, Courtier J, Phelps A, Copp HL, MacKenzie JD. Scrotal swelling in the neonate. J Ultrasound Med 2015;34:495–505.ArticlePubMedPMC
- 2. Oberlin DT, Cheng EY. Management of pediatric pyocele using percutaneous imaging-guided aspiration. Int J Surg Case Rep 2015;16:119–21.ArticlePubMedPMC
- 3. Kraft KH, Lambert SM, Snyder HM 3rd, Canning DA. Pyocele of the scrotum in the pediatric patient. J Pediatr Urol 2012;8:504–8.ArticlePubMed
- 4. Cetinkaya M, Buyukkale G, Payasli M, Ozbek S, Kavuncuoglu S. An unusual cause of bilateral scrotal abscess in a preterm infant: Candida albicans. Braz J Infect Dis 2013;17:260–2.ArticlePubMedPMC
- 5. Jones WG, Deeths HJ. Infected hydrocele in neonate. Urology 1975;5:526–7.ArticlePubMed
- 6. Terentiev V, Dickman E, Zerzan J, Arroyo A. Idiopathic infant pyocele: a case report and review of the literature. J Emerg Med 2015;48:e93–6.ArticlePubMed
- 7. Park SJ, Lee HK, Hong HS, Kim HC, Kim DH, Park JS, et al. Hydrocele of the canal of Nuck in a girl: ultrasound and MR appearance. Br J Radiol 2004;77:243–4.ArticlePubMed
- 8. Kim JY, Lim JH, Jung JY, Kim ER, Lee KC, Kang YM, et al. A case of meconium hydrocele presenting as inguinal mass in a female newborn. J Korean Soc Neonatol 2005;12:127–32.
- 9. Schalamon J, Ainoedhofer H, Schleef J, Singer G, Haxhija EQ, Höllwarth ME. Management of acute scrotum in children: the impact of Doppler ultrasound. J Pediatr Surg 2006;41:1377–80.ArticlePubMed
- 10. Slavis SA, Kollin J, Miller JB. Pyocele of scrotum: consequence of spontaneous rupture of testicular abscess. Urology 1989;33:313–6.ArticlePubMed
- 11. Kutin ND, Schwartz DL, So HB, Becker JM. Idiopathic infant pyoceles. J Pediatr Surg 1986;21:441–2.ArticlePubMed
References
Figure & Data
References
Citations

- Neonatal pyocele originating from a urinary tract infection: a case report
Zahra Jamali, Mohammad Shafie’ei, Najmeh Soltani Nejad
Journal of Medical Case Reports.2024;[Epub] CrossRef

 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine

 PubReader
PubReader ePub Link
ePub Link Cite
Cite






