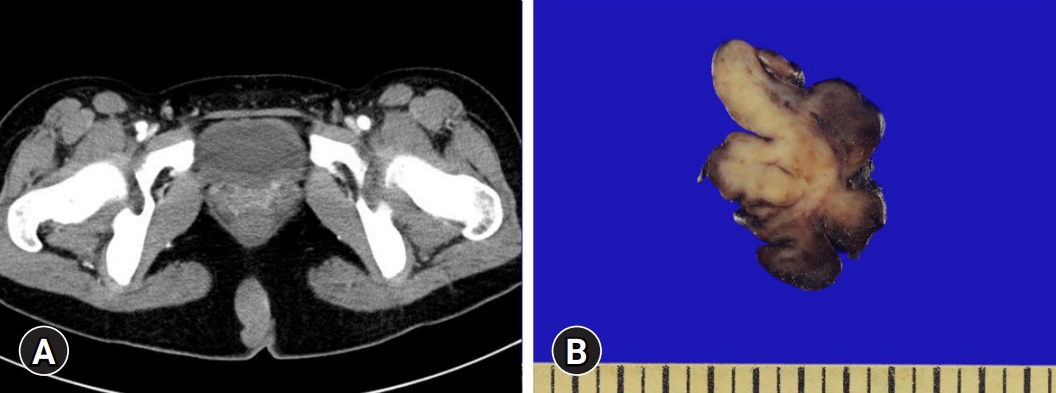
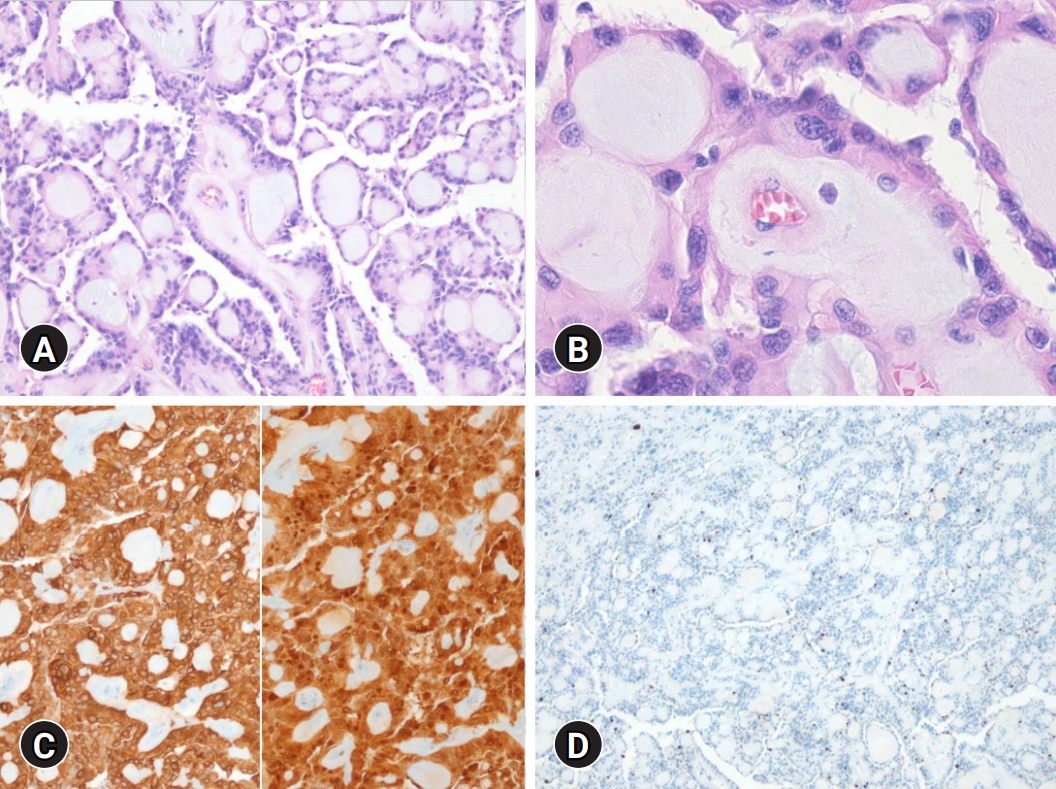
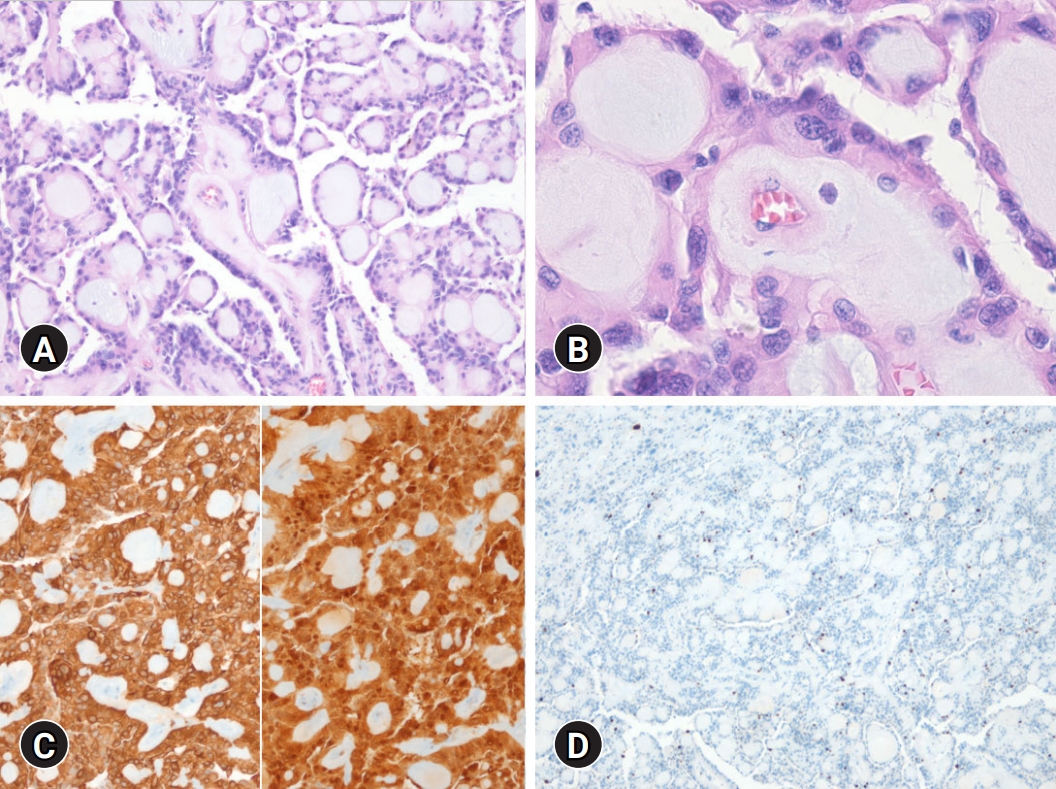
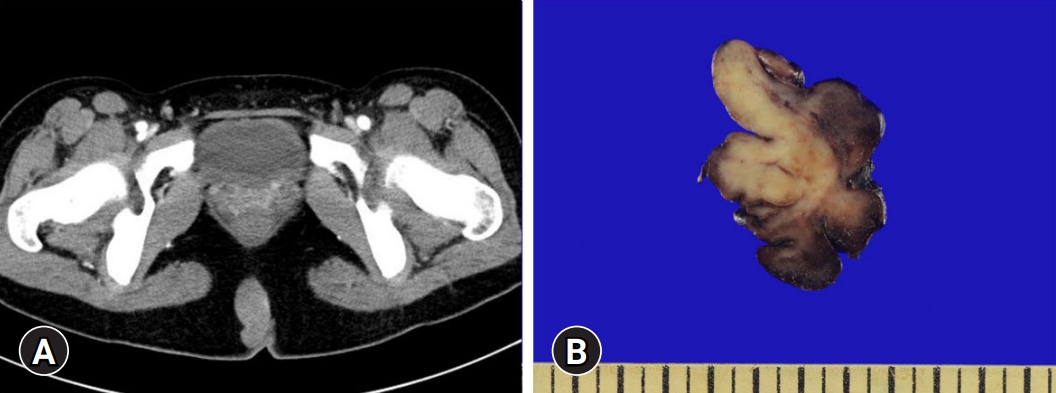
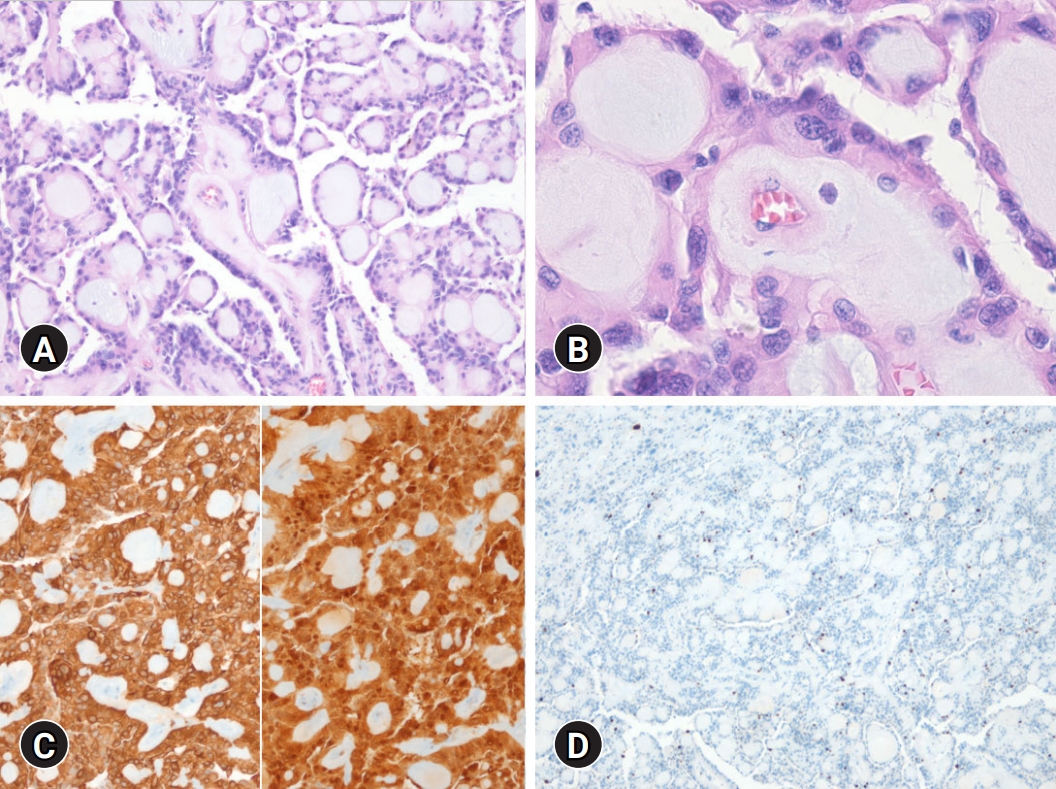
A 16-year-old female visited our out-patient clinic complaining of a mass near the anus developed over 6 months. She had no pain, tenderness, or incontinence. On physical examination, a few nodules were palpable near the anus, with no redness or discharge. Suspecting pilonidal disease and considering her attendance at school, the patient was prescribed antibiotics and surgery was planned during her vacation. Two months later, she underwent computed tomography which revealed a well-demarcated solid mass in the intragluteal fold area, which did not show any connection to the sacrum (Fig. 1A). These findings suggested tumors such as extraspinal sacrococcygeal myxopapillary ependymoma (ESME) rather than inflammatory changes. Elective surgery was performed, which revealed a multilobulated fleshy mass, measuring approximately 5.9×3.6 cm (Fig. 1B). On histologic examination, the tumor was well-demarcated by a fibrous capsule and composed of papillary structures with fibrovascular cores and myxoid materials, with relatively monomorphic tumor cells arranged along the papillary wall. In some areas, focal pleomorphic cells were identified but the highest mitotic count was 1/mm2. No necrosis or microvascular proliferation was observed. Immunohistochemical staining for GFAP and S100 protein was positive for tumor cells, but cytokeratin was negative and the Ki-67 index was less than 1% (Fig. 2). These features were consistent with ESME. On follow-up, brain and spine magnetic resonance imaging showed no metastasis or recurrence.
ESME is a rare glial tumor, and presented in an unusual location in our case. Since the first case reported by Mallory [1], less than 50 cases occurring in childhood have been reported in the literature [2]. Because of its rarity, the tumor is sometimes misdiagnosed as pilonidal abscess or detected only after treatment, including antibiotics or percutaneous aspiration [3,4].
Myxopapillary ependymoma (ME) has some unique histologic features [5]. The tumor is usually well-demarcated and has a papillary arrangement; tumor cells with relatively monomorphic nuclei having eosinophilic cytoplasm cover the surface of the papillary structures. Inside the papillary structure, is a small delicate vascular core with myxohyaline material. These histologic features are prototypic so that diagnosis usually does not require additional tools. The tumor cells are positive for GFAP and S100 protein. Dot-like epithelial membrane antigen positivity usually identified in other types of ependymoma is absent in ME. It is classified as anaplastic ME when the tumor demonstrates aggressive features (two or more of the following criteria: >2 mitosis/mm2, ≥10% Ki-67 index, microvascular proliferation, and necrosis). Recent molecular studies have revealed that the methylation profile can distinguish ME from other ependymomas [5].
There is no consensus on standardized therapy for ESME, but complete excision is recommended [2]. Radiotherapy can improve progression-free survival in spinal ependymoma and a similar result can be expected in ESME, especially in unresectable or partially excised cases; however, further investigations are required. According to the latest 2021 World Health Organization Classification of central nervous system tumors, the grade of ME was changed to 2 from 1 because it has a recurrence rate similar to conventional spinal ependymoma; therefore, more active treatment should be considered for patients with ME [5].
Notes
-
Ethical statements
This study was approved by the Institutional Review Board (IRB) of the Yeungnam University Hospital (IRB No: YUMC 2022-04-052). Informed consent was waived because of the retrospective nature of the case report.
-
Conflicts of interest
Mi Jin Gu has been an editorial board member of Journal of Yeungnam Medical Science since 2014. She was not involved in the review process of this manuscript. There is no other conflicts of interest to declare.
-
Funding
None.
-
Author contributions
Conceptualization, Formal analysis: MK, MJG; Methodology, Investigation, Data curation: MK; Supervision: MJG; Writing-original draft: MK; Writing-review & editing: MK, MJG.
Fig. 1.(A) Computed tomography scan revealing a well-demarcated mass in intragluteal fold area without connection to the sacrum. (B) Gross picture of extraspinal sacrococcygeal myxopapillary ependymoma. The mass shows a lobular growth pattern and fibrotic texture.
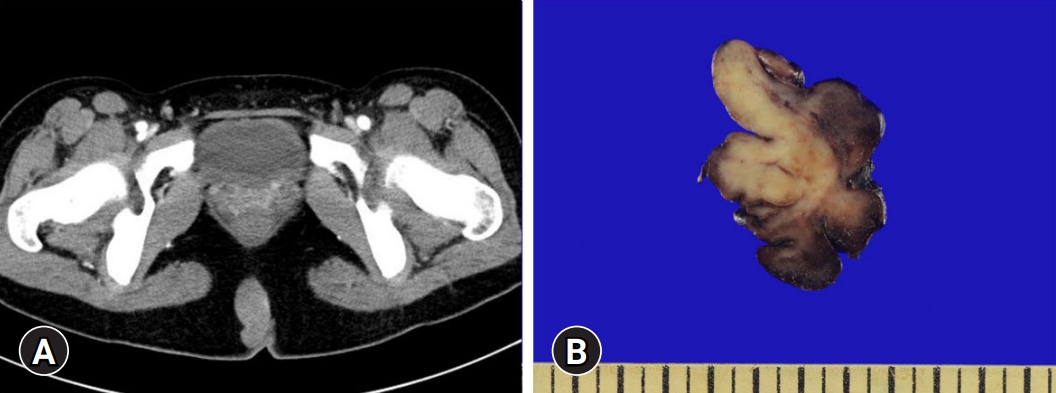
Fig. 2.(A) Microscopic examination shows a tumor composed of papillary structure with myxohyaline material. (B) Relatively monomorphic cuboidal cells are arranged around the myxopapillary structure (hematoxylin and eosin stain, ×100 [A] and ×400 [B]). (C) The tumor cells are positive for GFAP (left) and S100 protein (right). (D) Ki-67 immunohistochemical stain shows less than 1% nuclear positivity (immunohistochemical stain, ×100 [C] and x40 [D]).
References
- 1. Mallory FB. Three gliomata of ependymal origin; two in the fourth ventricle, one subcutaneous over the coccyx. J Med Res 1902;8:1–10. 1.PubMedPMC
- 2. Fabozzi F, Ceccanti S, Cacchione A, Colafati GS, Carai A, Crocoli A, et al. Pediatric extraspinal sacrococcygeal ependymoma: report of two cases and literature review. Diagnostics (Basel) 2021;11:1680.ArticlePubMedPMC
- 3. Kelly A, Nally D, Crowther S, Kavanagh D. Subcutaneous sacrococcygeal myxopapillary ependymoma misdiagnosed as pilonidal disease. BMJ Case Rep 2020;13:e231639.ArticlePubMedPMC
- 4. McEachron KR, Gaertner WB. Extradural sacrococcygeal subcutaneous ependymoma misdiagnosed as pilonidal disease: case report and review of the literature. J Surg Case Rep 2016;2016:rjw121.ArticlePubMedPMC
- 5. WHO Classification of Tumours Editorial Board. Central nervous system tumors. WHO Classification of Tumours, 5th ed. Lyon: International Agency for Research on Cancer; 2021.
Citations
Citations to this article as recorded by


 , Mi Jin Gu
, Mi Jin Gu


 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine PubReader
PubReader ePub Link
ePub Link Cite
Cite