PubMed Central, CAS, DOAJ, KCI

Articles
- Page Path
- HOME > J Yeungnam Med Sci > Volume 40(2); 2023 > Article
-
Case report
Transient osteoporosis of the hip with a femoral neck fracture during follow-up: a case report -
Yusuke Tabata1,4
 , Shuhei Matsui2
, Shuhei Matsui2 , Masabumi Miyamoto3
, Masabumi Miyamoto3 , Koichiro Omori1
, Koichiro Omori1 , Yoichiro Tabata1
, Yoichiro Tabata1 , Tokifumi Majima4
, Tokifumi Majima4
-
Journal of Yeungnam Medical Science 2023;40(2):212-217.
DOI: https://doi.org/10.12701/jyms.2022.00479
Published online: September 26, 2022
1Department of Orthopedic Surgery, Mitsuhashi Hospital, Chiba, Japan
2Department of Orthopedic Surgery, Musashino General Hospital, Kawagoe, Japan
3Department of Orthopedic Surgery, Sekishindo Hospital, Kawagoe, Japan
4Department of Orthopedic Surgery, Nippon Medical School Hospital, Tokyo, Japan
- Corresponding author: Yusuke Tabata, MD, PhD Department of Orthopedic Surgery, Mitsuhashi Hospital, Kameicho, Chuo-ku, Chiba 260-0011, Japan Tel: +81-432248201 • Fax: +81-432248205 • E-mail: yusuketabata3@gmail.com
Copyright © 2023 Yeungnam University College of Medicine, Yeungnam University Institute of Medical Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
- We report a case of transient osteoporosis of the hip with a femoral neck fracture found during follow-up. A 53-year-old man presented with left hip pain without trauma. The pain did not improve after 2 weeks and he was brought to our hospital by ambulance. Magnetic resonance imaging (MRI) of the left hip joint showed diffuse edema in the bone marrow, which was identified by low signal intensity on T1-weighted images, high signal intensity on T2-weighted images, and increased signal intensity on short tau inversion recovery. This edema extended from the femoral head and neck to the intertrochanteric area. He was diagnosed with transient osteoporosis of the left hip. Rest gradually improved his pain; however, 3 weeks later, his left hip pain worsened without trauma. X-ray, computed tomography, and MRI results of the hip joint demonstrated a left femoral neck fracture, and osteosynthesis was performed. Differential diagnoses included avascular necrosis of the femoral head, infection, complex regional pain syndrome, rheumatoid arthritis, leukemia, and other cancers. Transient osteoporosis of the hip generally has a good prognosis with spontaneous remission within a few months to 1 year. However, a sufficient length of follow-up from condition onset to full recovery is necessary to avoid all probable complications such as fractures.
- Transient osteoporosis of the hip (TOH) is a rare disease that was first reported in 1959 in three pregnant women who had strong unilateral or bilateral hip pain [1]. TOH generally occurs in middle-aged men and pregnant women in their last trimester [2-4]. Its etiology is unknown; however, it is suspected that ischemia in the femoral head could be involved in the onset of TOH [5-7]. Differential diagnosis includes avascular necrosis of the femoral head, infection, complex regional pain syndrome, rheumatoid arthritis, leukemia, and other cancers. TOH is conventionally a disease with a good prognosis and spontaneous remission within a few months to 1 year. We report a case of TOH where a femoral neck fracture later occurred without trauma, and osteosynthesis was performed.
Introduction
- Ethical statements: Written informed consent was obtained from the patient for this case report. This study was approved by the Institutional Review Board (IRB) of Musashino General Hospital (IRB No: 12).
- A 53-year-old man presented with left hip pain without trauma that had persisted for 2 weeks. After the pain did not subside, he was brought to our hospital by ambulance. He had schizophrenia and epilepsy resulting from a previous head injury. He drank approximately 1.5 L of beer every day and had smoked 20 cigarettes per day for 37 years.
- On the first admission, he had difficulty walking due to severe left hip pain. The blood examination was normal. His left hip joint demonstrated painful limitations in passive range of motion. Patrick’s test was positive.
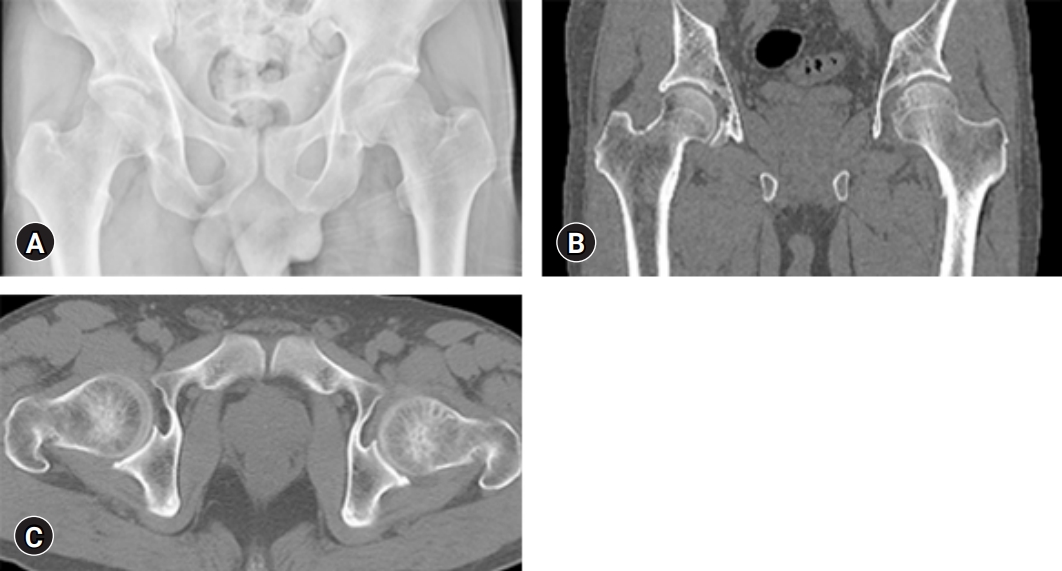
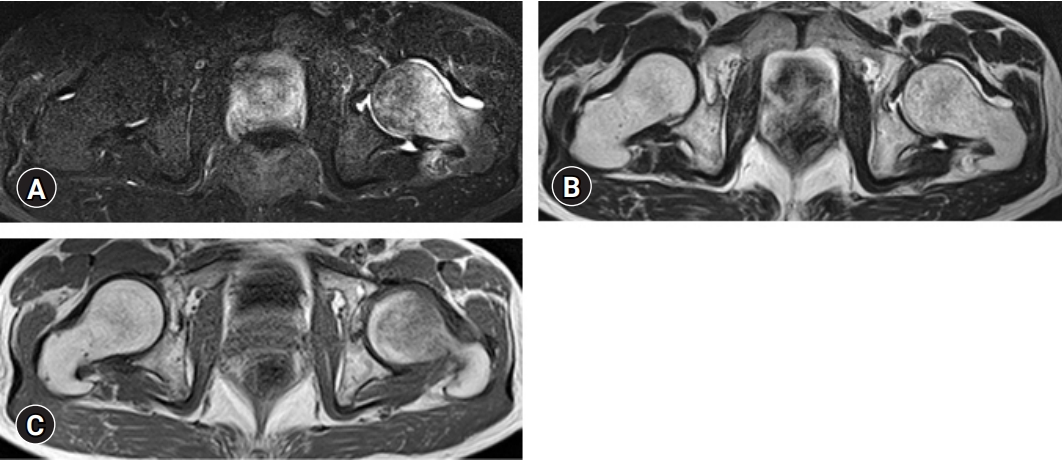
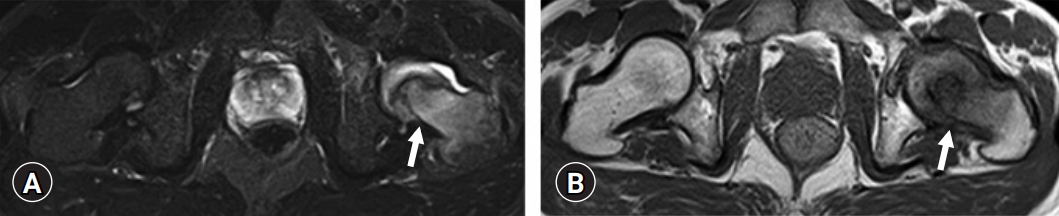
- X-ray and computed tomography (CT) revealed no obvious fracture (Fig. 1). Magnetic resonance imaging (MRI) showed diffuse edema in the bone marrow, which was identified by low signal intensity on T1-weighted images, high signal intensity on T2-weighted images, and increased signal intensity on short tau inversion recovery (STIR). This edema extended from the femoral head and neck to the intertrochanteric area (Figs. 2, 3).
- We prescribed rest and non-weight bearing for him; however, he did not follow our instructions due to his psychological condition. His pain gradually improved and he was discharged from our hospital using crutches.
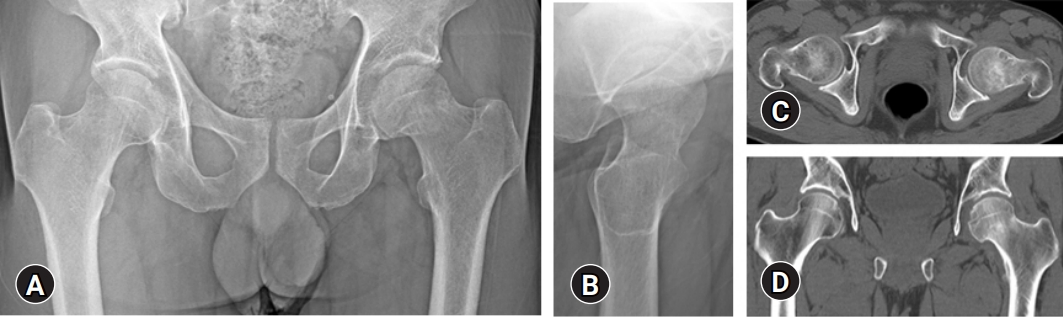
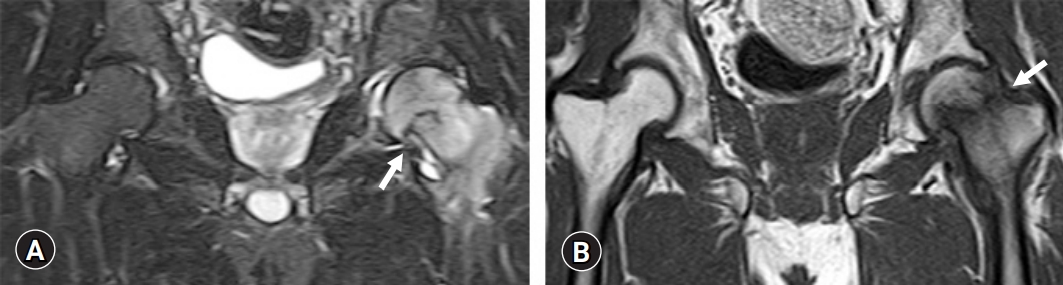
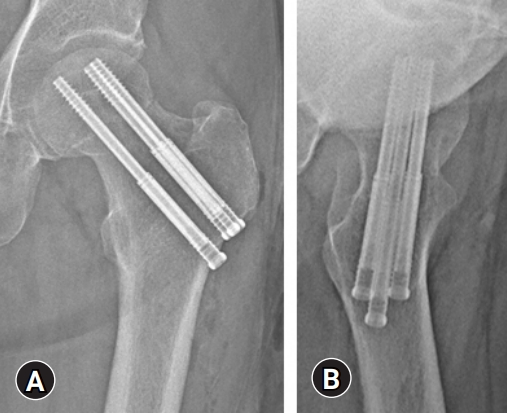
- Three weeks later, his left hip pain worsened without trauma and he visited our hospital again. X-ray, CT scan, and MRI of the hip joint demonstrated a left femoral neck fracture (Garden stage Ⅱ) (Figs. 4–6), and osteosynthesis (Prima Hip Screw System, Japan Medical Dynamic Marketing, Inc., Tokyo, Japan) was performed (Fig. 7).
Case
- TOH generally affects middle-aged men and pregnant women in their last trimester [2-4]. It is usually bilateral in pregnant women and unilateral in middle-aged men [8]. The cause and pathogenesis of TOH remain unclear; however, the most dominant theory implicates femoral head ischemia due to venous obstruction as the cause [5-7]. On examination, bone biopsies of patients with TOH showed increased numbers of erythrocytes, suggesting the presence of venous stasis [5]. Furthermore, Orth and Anagnostakos [9] reported that decreased concentrations of fibrinolytic agents and increased concentrations of thrombophilia markers in TOH patients could potentially cause venous obstruction. Risk factors for TOH include trauma, a history of steroid use, consumption of alcohol, smoking, low testosterone levels, low vitamin D levels, osteogenesis imperfecta, hypothyroidism, and hypophosphatasia [10-13]. In this case, smoking and alcohol were mentioned as risk factors.
- MRI is the most powerful tool for the diagnosis of TOH and usually shows low signal intensity on T1-weighted images, high signal intensity on T2-weighted images, and increased signal intensity on STIR, reflecting bone marrow edema.
- TOH typically has a good prognosis with spontaneous remission occurring within a few months to 1 year. Methods for joint preservation, including restricted weight bearing, are the first-line therapy. As alternative treatments, the use of bisphosphonates to inhibit bone resorption and the use of teriparatide as an osteoanabolic agent were reported to provide successful outcomes [14-17]. Additionally, hyperbaric oxygen therapy was reported to potentially accelerate recovery in TOH patients, although the effects were not statistically significant [18]. More recently, out of 15 TOH cases, 10 underwent hip drilling for core decompression while five underwent conservative therapy. An investigation of the time to full recovery revealed that hip drilling required a median of 5.8 weeks while conservative therapy required 48.3 weeks, demonstrating the validity of hip drilling as a treatment modality [19].
- In the present case, regarding our recommendations to avoid bearing weight, the patient was nonadherent due to his poor mental health; therefore, it was assumed that the constant stress of weight bearing caused the femoral neck fracture. In fact, the fracture pattern in this case originated in the lower part of the femoral neck and is considered to be a pathological condition similar to insufficient fracture secondary to TOH. Interestingly, Hadji et al. [20] demonstrated that out of 52 TOH patients, 12.1% sustained a hip fracture. Therefore, for patients with a high likelihood of fracture, it is necessary to provide thorough education, such as instructions not to apply a load to the lower limbs during a specified period. Prophylactic osteosynthesis may also be considered for patients expected to have a high likelihood of fracture. Considering these factors, a sufficient follow-up period from condition onset to full recovery is necessary to avoid as many complications as possible.
Discussion
-
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
-
Funding
None.
-
Author contributions
Conceptualization, Supervision: YT, TM; Data curation: YT, SM, MM; Formal analysis: SM, MM, KO, YT, TM; Investigation: YT; Writing-original draft: YT; Writing-review & editing: all authors.
Notes

- 1. Curtiss PH Jr, Kincaid WE. Transitory demineralization of the hip in pregnancy: a report of three cases. J Bone Joint Surg Am 1959;41-A:1327–33.ArticlePubMed
- 2. Van Wagenen K, Pritchard P, Taylor JA. Transient osteoporosis of the hip: a case report. J Can Chiropr Assoc 2013;57:116–22.PubMedPMC
- 3. Ma FY, Falkenberg M. Case reports: transient osteoporosis of the hip: an atypical case. Clin Orthop Relat Res 2006;445:245–9.ArticlePubMed
- 4. Asadipooya K, Graves L, Greene LW. Transient osteoporosis of the hip: review of the literature. Osteoporos Int 2017;28:1805–16.ArticlePubMedPDF
- 5. Rosen RA. Transitory demineralization of the femoral head. Radiology 1970;94:509–12.ArticlePubMed
- 6. Plenk H Jr, Hofmann S, Eschberger J, Gstettner M, Kramer J, Schneider W, et al. Histomorphology and bone morphometry of the bone marrow edema syndrome of the hip. Clin Orthop Relat Res 1997;(334):73–84.Article
- 7. Koo KH, Jeong ST, Jones JP Jr. Borderline necrosis of the femoral head. Clin Orthop Relat Res 1999;(358):158–65.Article
- 8. Manara M, Varenna M. A clinical overview of bone marrow edema. Reumatismo 2014;66:184–96.ArticlePubMedPDF
- 9. Orth P, Anagnostakos K. Coagulation abnormalities in osteonecrosis and bone marrow edema syndrome. Orthopedics 2013;36:290–300.ArticlePubMed
- 10. Diwanji SR, Cho YJ, Xin ZF, Yoon TR. Conservative treatment for transient osteoporosis of the hip in middle-aged women. Singapore Med J 2008;49:e17–21.PubMed
- 11. Daniel RS, Farrar EK, Norton HR, Nussbaum AI. Bilateral transient osteoporosis of the talus in pregnancy. Osteoporos Int 2009;20:1973–5.ArticlePubMedPDF
- 12. Jennings PE, O’Malley BP, Griffin KE, Northover B, Rosenthal FD. Relevance of increased serum thyroxine concentrations associated with normal serum triiodothyronine values in hypothyroid patients receiving thyroxine: a case for “tissue thyrotoxicosis”. Br Med J (Clin Res Ed) 1984;289:1645–7.ArticlePubMedPMC
- 13. Dunstan CR, Evans RA, Somers NM. Bone death in transient regional osteoporosis. Bone 1992;13:161–5.ArticlePubMed
- 14. Flores-Robles BJ, Sanz-Sanz J, Sanabria-Sanchinel AA, Huntley-Pascual D, Andréu Sánchez JL, Campos Esteban J, et al. Zoledronic acid treatment in primary bone marrow edema syndrome. J Pain Palliat Care Pharmacother 2017;31:52–6.ArticlePubMed
- 15. Emad Y, Ragab Y, El-Shaarawy N, Rasker JJ. Transient osteoporosis of the hip, complete resolution after treatment with alendronate as observed by MRI description of eight cases and review of the literature. Clin Rheumatol 2012;31:1641–7.ArticlePubMedPDF
- 16. Kibbi L, Touma Z, Khoury N, Arayssi T. Oral bisphosphonates in treatment of transient osteoporosis. Clin Rheumatol 2008;27:529–32.ArticlePubMedPDF
- 17. Schapira D, Braun Moscovici Y, Gutierrez G, Nahir AM. Severe transient osteoporosis of the hip during pregnancy: successful treatment with intravenous biphosphonates. Clin Exp Rheumatol 2003;21:107–10.PubMed
- 18. Yagishita K, Jinno T, Koga D, Kato T, Enomoto M, Kato T, et al. Transient osteoporosis of the hip treated with hyperbaric oxygen therapy: a case series. Undersea Hyperb Med 2016;43:847–54.PubMed
- 19. Bashaireh KM, Aldarwish FM, Al-Omari AA, Albashaireh MA, Hajjat M, Al-Ebbini MA, et al. Transient osteoporosis of the hip: risk and therapy. Open Access Rheumatol 2020;12:1–8.ArticlePubMedPMC
- 20. Hadji P, Boekhoff J, Hahn M, Hellmeyer L, Hars O, Kyvernitakis I. Pregnancy-associated transient osteoporosis of the hip: results of a case-control study. Arch Osteoporos 2017;12:11.ArticlePubMedPDF
References
Figure & Data
References
Citations

- Hip effusion/synovitis influences results after multiple drilling core decompression for bone marrow edema syndrome of hip
Hua-zhang Xiong, Yan-li Peng, Yu-hong Deng, Ying Jin, Ming-hong Tu, Shu-hong Wu
BMC Surgery.2023;[Epub] CrossRef

 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine PubReader
PubReader ePub Link
ePub Link Cite
Cite








