PubMed Central, CAS, DOAJ, KCI

Articles
- Page Path
- HOME > J Yeungnam Med Sci > Volume 40(3); 2023 > Article
-
Case report
Morgagni-Stewart-Morel syndrome presenting with neurological symptoms: a case report -
Bünyamin Tosunoğlu
 , Nazlıcan Ergin
, Nazlıcan Ergin , Nilay Kaya
, Nilay Kaya , Levent Ertuğrul İnan
, Levent Ertuğrul İnan
-
Journal of Yeungnam Medical Science 2023;40(3):308-310.
DOI: https://doi.org/10.12701/jyms.2022.00675
Published online: December 1, 2022
Department of Neurology, Ankara Training and Research Hospital, Ankara, Turkey
- Corresponding author: Bünyamin Tosunoğlu, MD Department of Neurology, Ankara Training and Research Hospital, Hacettepe, Ulucanlar Cd. No: 89, Altındağ 06230, Ankara, Turkey Tel: +90-507-278-28-66 • Fax: +90-312-363-33-96 • E-mail: bunyamin.tosunoglu@saglik.gov.tr
Copyright © 2023 Yeungnam University College of Medicine, Yeungnam University Institute of Medical Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 2,729 Views
- 87 Download
Abstract
- Morgagni-Stewart-Morel (MSM) syndrome is characterized by the thickening of the frontal bone of the skull (hyperostosis frontalis interna) obesity, neurological symptoms, and hypertrichosis. We present the case of a 76-year-old patient who complained of confusion, extreme irritability, and headache and was diagnosed with MSM based on examination, imaging, and test results.
- Morgagni-Stewart-Morel (MSM) syndrome is characterized by the thickening of the frontal bone of the skull (hyperostosis frontalis internal), obesity, neurological symptoms, and hypertrichosis [1-3]. In addition, diabetes, hyperparathyroidism, and other endocrine problems may accompany this condition. Headache, dizziness, atrophy of the frontal lobe, a decreased sense of sight and smell, parkinsonism, anxiety, depression, confusion, cognitive disorders, and seizures may accompany the neurological symptoms [4,5]. The etiology of MSM syndrome is not fully understood. The syndrome was described in 1719 by pathologist Giovanni Battista Morgagni, in 1928 by neurologist Roy Mackenzie Stewart, and in 1930 by psychiatrist Ferdinand Morel [1,2,4].
Introduction
- Ethical statements: Our institution does not require Institutional Review Board approval for case reports. Informed consent was obtained from the patient.
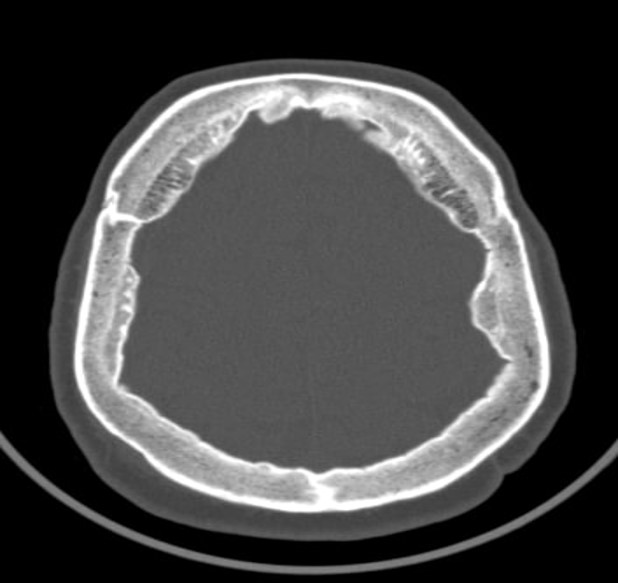
- A 76-year-old female patient was brought to the emergency department with confusion, dizziness, and extreme nervousness that had started 2 days earlier. In the anamnesis, it was found that she had a headache for years, did not enjoy life occasionally, and was extremely nervous. On physical examination, the patient’s general condition was good, body temperature was normal, and vital signs were stable. On neurological examination, there were no signs other than orientation and limited cooperation, and the patient did not have neck stiffness. Other system examinations were normal. No acute pathology was detected on brain computed tomography (CT) and magnetic resonance imaging (MRI) performed in the emergency department. An axial cranial CT scan showed bilateral thickening of the inner table of the frontal bone (Fig. 1).
- She was administered irbesartan 150 mg/day for hypertension. The patient had no history of trauma or febrile illness and was admitted to our hospital for further examination and treatment. Routine blood tests, whole blood, vitamin B12 levels, ammonia, thyroid function tests, hemoglobin A1c, erythrocyte sedimentation rate, serum electrophoresis, autoantibody screening (antinuclear antibody, anti-SSA, and anti-SSB), antithyroid antibodies, syphilis serology (fluorescent treponemal antibody), and Schirmer’s test were normal. Enzyme-linked immunosorbent assay tests and pathergy tests for Behçet disease were negative. The complete urinalysis results were within normal limits. Screening for viral meningitis and Brucella yielded negative results.
- The patient’s blood biochemistry results showed high urea, high parathormone (82.7 ng/L; range, 15–65 ng/L), and low 25-hydroxyvitamin D levels. There were mild signs of hirsutism and progesterone, testosterone, 17β-estradiol levels were normal. A score of 19 was obtained on the Mini-Mental State Examination (MMSE). Growth hormone and somatomedin C indicative of acromegaly were within normal limits. The patient was referred to endocrinology, and vitamin D treatment was administered.
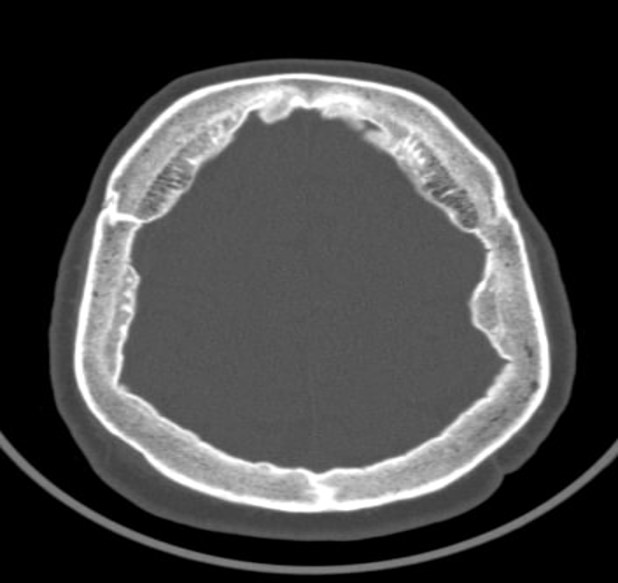
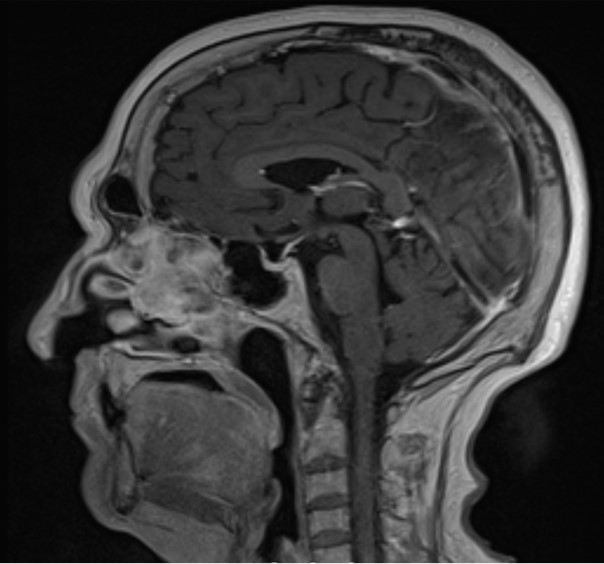
- Brain MRI of the patient revealed no findings other than hyperostosis frontalis interna. Sagittal T1-weighted MRI and an axial section cranial scan showed nodular bony overgrowth involving the frontal endocranium (Fig. 2). The patient’s body mass index (BMI) was 30 kg/m2. Electroencephalography (EEG) revealed seizure activity, and our patient was started on levetiracetam 500 mg twice a day. No significant pathology was found in the breast examination for Paget disease or a bone survey X-ray taken for lytic lesions.
- The patient was diagnosed with MSM syndrome based on anamnesis, examination findings, and imaging results. She was discharged with the recommendation of a neurology outpatient follow-up, with treatment for her current complaints.
Case
- MSM syndrome was first described by Giovanni Battista Morgagni in 1719 as a thickening of the inner layer of the skull in an obese female patient with hirsutism and hyperostosis frontalis interna observed during autopsy. In 1928, Stewart reported three cases found during autopsy. In 1930, Morel reported the first living case. MSM syndrome presents with endocrinological, metabolic, and neuropsychiatric symptoms [1-5].
- Our patient had extreme irritability, confusion, and headaches. Seizure activity was also detected in the EEG results. Our patient had hypertension but did not have diabetes. She showed signs of hirsutism and a BMI of 30 kg/m2. Hyperostosis frontalis was detected in the imaging results of our patient, and the laboratory findings revealed high urea, high parathormone, and low vitamin D levels. Fibrous dysplasia, acromegaly, and Paget disease were excluded in the differential diagnosis. The first MMSE score was 19 points, and the repeated MMSE score was 26 points. MSM syndrome is rare and usually occurs in women. The mean age of onset is 45 years. Reported cases in literature are predominantly women [1–3]. The patient was a 76-year-old female. Although the pathophysiology of MSM syndrome has not been clearly determined, it is believed to be related to long-term exposure to estrogen, obesity, high leptin levels, and genetics [3,4]. Genetic transmission is believed to be autosomal dominant.
- Treatment of MSM syndrome is symptom-based and usually includes weight-control medications, as well as diet and lifestyle changes. Seizures and headaches associated with hyperostosis frontalis interna are treated using standard medications [1,4,5]. As a result, MSM syndrome should be considered in patients presenting with similar symptoms. Thorough anamnesis should be taken, radiological imaging performed, metabolic parameters tested, and symptomatic treatment administered after the diagnosis is made.
Discussion
-
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
-
Funding
None.
-
Author contributions
Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Visualization, Investigation, Resources, Software, Supervision, Validation: all authors; Writing-original draft, all authors; Writing-review & editing, all authors.
Notes
- 1. Attanasio F, Granziera S, Giantin V, Manzato E. Full penetrance of Morgagni-Stewart-Morel syndrome in a 75-year-old woman: case report and review of the literature. J Clin Endocrinol Metab 2013;98:453–7.ArticlePubMed
- 2. Abainou L, El Jadi H, El Hadri S, Baizri H. Morgagni-Stewart-Morel syndrome: a new case. Case Rep Int 2019;8:100070Z06LA2019.Article
- 3. Doğan E, Mouline M. Morgagni-Stewart-Morel syndrome: case report. Turk J Clin Lab 2019;10:434–6.Article
- 4. Nallegowda M, Singh U, Khanna M, Yadav SL, Choudhary AR, Thakar A. Morgagni Stewart Morel syndrome--additional features. Neurol India 2005;53:117–9.ArticlePubMed
- 5. Kishore B, Singh MM, Seth HC, Hazra DK, Trehon OP, Prakash C. Morgagni’s syndrome: a case report. J Indian Med Assoc 1972;58:376–8.PubMed
References
Figure & Data
References
Citations


 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine PubReader
PubReader ePub Link
ePub Link Cite
Cite