Indexed in: ESCI, Scopus, PubMed,
PubMed Central, CAS, DOAJ, KCI
PubMed Central, CAS, DOAJ, KCI
FREE article processing charge

Articles
- Page Path
- HOME > J Yeungnam Med Sci > Ahead-of print > Article
-
Focused Review article
The prevalence and prevention strategies of pediatric obesity: a narrative review -
Mi Seon Lee

-
DOI: https://doi.org/10.12701/jyms.2024.00346
Published online: July 5, 2024
Department of Pediatrics, Soonchunhyang University Gumi Hospital, Soonchunhyang University College of Medicine, Korea
- Corresponding author: Mi Seon Lee, MD, PhD Department of Pediatrics, Soonchunhyang University Gumi Hospital, Soonchunhyang University College of Medicine, 179 1gongdan-ro, Gumi 39371, Korea Tel: +82-54-468-9233 • Fax: +82-54-463-7504 • E-mail: skymerrong@gmail.com
• Received: April 4, 2024 • Revised: May 27, 2024 • Accepted: May 28, 2024
© 2024 Yeungnam University College of Medicine, Yeungnam University Institute of Medical Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 166 Views
- 13 Download
Abstract
- Pediatric obesity has rapidly increased globally over the past few decades, including in Korea. We aimed to discuss trends in the prevalence of pediatric obesity and effective prevention strategies. Its prevalence has markedly increased in most high-income nations. According to recent reports, this increase has slowed in developed countries, but the levels remain alarmingly high. In Korea, the rate of pediatric obesity has surged notably since the 1990s; however, since the 2000s, this increase has become more gradual. According to recently published 2017 growth charts, the prevalence of pediatric obesity in Korea varies slightly depending on the data source. The National School Health Examination data showed that pediatric obesity gradually increase from 11.5% in 2014 to 15.1% in 2019, and after the coronavirus disease 2019 pandemic, it sharply increased to 19% in 2021. Based on data from the Korea National Health and Nutrition Examination Survey, the prevalence of pediatric obesity gradually increased from 10.8% in 2017 to 13.6% in 2019. This trend, which accelerated sharply to 15.9% in 2020 and 19.3% in 2021, was especially severe in boys and older children. Pediatric obesity not only affects health during childhood but also increases the risk of developing obesity and associated health conditions in adulthood. Despite ongoing research on treatment options, obesity prevention and control remain challenging. Hence, prioritizing early intervention and prevention of pediatric obesity through healthy eating habits and lifestyles is crucial. This requires intervention at the individual, family, school, and community levels.
- The incidence of pediatric obesity has steadily increased worldwide over the past several decades and has emerged as a significant public health issue [1,2]. It is primarily a lifestyle-related disease caused by an imbalance between energy intake and expenditure, leading to excessive fat accumulation [3]. Although numerous treatment methods for obesity are being investigated, effectively managing obesity can be challenging once it develops [4]. Importantly, a significant proportion of adult obesity originates in childhood, with infants and children who are obese having a higher likelihood of remaining obese into adulthood [5,6]. Moreover, beyond the health issues associated with pediatric obesity, the resulting adult obesity and its comorbidities lead to substantial medical expenses [7]. Knowledge of the prevalence of pediatric obesity would help accurately determine the extent of the current burden and facilitate the establishment of appropriate treatment and prevention measures. In this review, we aimed to discuss trends in the prevalence of pediatric obesity and effective prevention strategies.
Introduction
- 1. Trends in the prevalence of pediatric obesity
- The global prevalence of pediatric obesity has markedly surged in recent decades. Over the last 30 years, the incidence of children who are overweight or obese has increased substantially in numerous high-income nations. The regions with the largest increases in such incidences are East Asia, the Middle East and North Africa, South Asia, and high-income English-speaking regions [8,9]. In the United States, the average weight of children increased by more than 5 kg during this period, resulting in approximately one-third of children being classified as overweight or obese [1,10]. Although a plateau in the trend of pediatric obesity rates was observed in developed countries such as northwestern Europe, high-income English-speaking countries, and the Asia-Pacific region during the early 2000s, these rates have remained elevated [11,12], and the occurrence of severe obesity has been increasing [13]. Additionally, overweight and obesity, which were thought to be problems in high-income countries, are now on the rise in low- and middle-income countries [9]. Southeast Asia, South Africa, and Latin America are experiencing a relatively rapid transition from underweight to overweight and obese populations. In Africa, the number of overweight children under 5 years of age has increased by almost 23% since 2000; in 2022, almost half of the children under 5 years of age who were overweight or obese lived in Asia. The proportional increase over the past decade was the lowest in high-income regions (on average, 30%–50% per decade) and the highest in South Africa (approximately 400% per decade) [8,9].
- The prevalence of obesity varies depending on the definition of obesity, whether it is based on obesity grade or body mass index (BMI). Generally, BMI is used as a criterion to determine obesity. This varies depending on sex, age, and population group; thus, comparisons are made using standards specific to each population group. Differences may also arise depending on the time at which the standard weight is used. The prevalence of obesity in children and adolescents in Korea is analyzed based on the Korean national growth charts for children and adolescents published in 1967, 1975, 1985, 1998, 2007, and 2017 [14-19].
- According to the 1998 growth charts, a survey conducted on school-aged children in Seoul revealed a higher prevalence of underweight than obesity in children in 1979 and 1981. However, with the gradual increase in BMI, the prevalence of obesity among boys increased from 6.2% in 1988 to 11.0% in 1997 and further to 17.9% in 2002. Similarly, the prevalence among girls increased consistently from 6.5% in 1988 to 9.0% in 1997, eventually reaching 10.9% in 2002. As Korean society has advanced, the number of individuals who are obese has surpassed that of those who are underweight, and this disparity has widened over time. The incidence of obesity in children and adolescents, particularly in boys, has surged since the 1990s [20].
- Based on the 2007 growth charts, the prevalence of pediatric obesity increased approximately 1.7 times from 5.8% in 1997 to 9.7% in 2005. Notably, there was an increasing trend among boys aged 13 to 18 years [21]. Although there were some differences depending on the data source and included age groups, the prevalence of obesity among children aged 6 to 18 years, based on the National School Health Examination (NSHE) data, increased from 8.7% in 2007 to 15.0% in 2017. Moreover, according to data from the Korea National Health and Nutrition Examination Survey (KNHANES), the prevalence of obesity among children aged 2 to 18 years increased slightly from 8.6% in 2001 to 9.8% in 2017. This increase was significant among both male students and high school students [22]. When severe obesity was defined as a BMI exceeding 120% of the 95th percentile, the prevalence of severe obesity in Korean individuals aged 2 to 19 years increased from 1.2% in 2001 to 2.1% in 2013 to 2014 according to KNHANES data. Notably, this increase was especially pronounced among adolescent boys in their teens [23,24].
- 2. Current status of overweight and obesity prevalence in Korea based on the 2017 growth charts
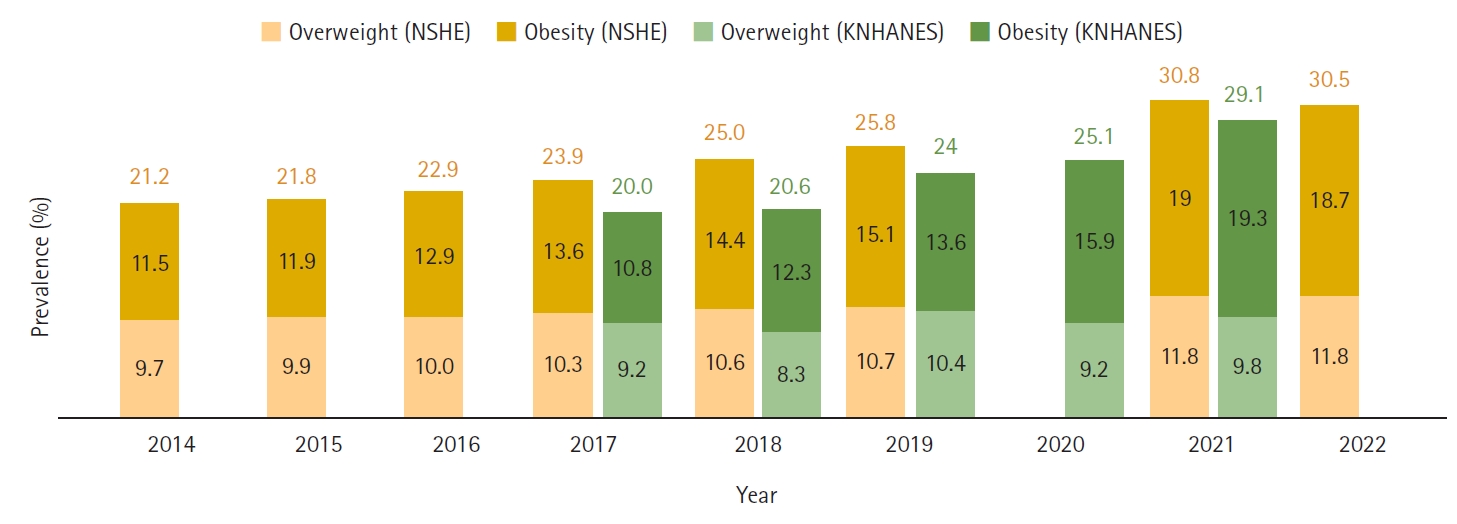
- The prevalence of childhood obesity has been evaluated using data from the NSHE, conducted annually by the Ministry of Education, and KNHANES, administered by the Ministry of Health and Welfare [25,26]. To accurately discern these trends, uniform standards must be consistently applied for comparison. However, analyzing historical data within a singular standard framework presents challenges. Consequently, our analysis aimed to elucidate the current trend in the prevalence of pediatric obesity in Korea by utilizing the most recently published standard reference (2017), which is categorized by age and height. Using the 2017 growth charts, KNHANES data from 2017 to 2021 and NSHE data from 2014 to 2022 were available (Fig. 1). In the 2007 growth charts, overweight was defined as BMI ≥85th percentile and <95th percentile, and obesity was defined as BMI ≥95th percentile or BMI ≥25 kg/m2 by age and sex [18]. In the new 2017 growth charts, the definition of overweight remained unchanged, but the definition of obesity was changed to BMI ≥95th percentile by sex and age [19].
- In the NSHE data from 2014 to 2022 (elementary, middle, and high school children), based on 2017 growth charts, there was a gradual increase yearly from 11.5% in 2014 to 15.1% in 2019. Owing to the coronavirus disease 2019 (COVID-19) pandemic, the survey was not conducted in 2020 because of the difficulty in securing a sufficient sample size, which then increased rapidly in 2021, reaching 19%. Based on the 2007 growth charts, the prevalence of pediatric obesity from 2014 to 2017 was 12.9%, 13.4%, 14.3%, and 15.0%, respectively [22]. The prevalences showed minor discrepancies compared with those based on the new 2017 growth charts. The prevalence increased with age, and boys exhibited a higher prevalence than girls (Table 1). Owing to the absence of height and weight measurements, data for children aged 6 to 9 years from KNHANES were omitted, leading to the exclusion of the initial period data. Furthermore, data spanning 2001 to 2009 were omitted because calculating the monthly age was not feasible. By utilizing the 2017 growth charts, there was a gradual increase in prevalence across the 5th to 7th cycles (5th period [2010–2012], 10.2%; 6th period [2013–2015], 10.3%; and 7th period [2016–2018], 11.6%) and a marked increase in the 8th period (2019–2021) to 16.2%. A steady annual increase was observed between 2017 and 2020, followed by a significant surge between 2020 and 2021. Moreover, the prevalence was notably higher in the 12 to 18-year age group than in the 6 to 11-year age group, with boys surpassing girls in prevalence, and the rate of increase was greater (Table 2).
- While the NSHE offers the benefit of a large sample size, it has a margin of error stemming from the variance in actual height and weight measurements across schools. Furthermore, it excludes children who are not enrolled in school. The KNHANES data are representative of the country and have the advantage of being measured by experts. Nonetheless, it has the disadvantage of a relatively small number of pediatric participants each year. Although slight variations in prevalence exist depending on the data source, the prevalence of obesity in Korea has gradually increased since the 2010s, exhibiting a sharp increase. This trend aligns with the reported plateauing of pediatric obesity prevalence in numerous developed countries, with the rapid escalation post-2020 likely attributable to lifestyle changes induced by the COVID-19 pandemic [27,28]. Both datasets were collected cross-sectionally; therefore, a nationwide longitudinal cohort study is warranted. In addition, unlike adults, pediatric obesity is defined by BMI percentiles by sex and age, showing differences in prevalence depending on the standard growth chart. To accurately examine the prevalence of recent growth and developmental trends, it is necessary to continuously update childhood growth charts in the future.
Changes in the prevalence of pediatric obesity
- Obesity in children and adolescents not only leads to comorbidities such as hypertension, dyslipidemia, diabetes, and nonalcoholic fatty liver disease but also contributes to mental and psychological issues, including depression and a negative self-image [29-34]. Furthermore, obesity in this demographic is highly likely to persist into adulthood, posing a risk for various diseases, including cardiovascular disease [35-37]. This situation incurs significant socioeconomic costs [38,39]. Therefore, to effectively address pediatric obesity, it is crucial to appropriately diagnose and evaluate comorbidities [40]. Obesity in childhood and adolescence is mainly caused by the consumption of cheap, energy-dense, and low-nutrition foods and drinks, along with a Western diet and commercial interests that lead to a sedentary lifestyle. Intrauterine and postnatal environments, a lack of sleep, and adverse childhood experiences also have an impact. These factors are modifiable [41,42]. The main approaches for treating obesity involve lifestyle modifications, medication therapy, and bariatric surgery in rare cases [34]. As it is difficult to obtain adequate and long-lasting outcomes once obesity develops, the main goal should be ensuring early prevention of pediatric obesity and improving healthy eating habits, physical activity, and living environment [40] (Table 3). Interventions at various levels, including individuals, families, schools, and society, are essential to achieve this goal [43].
- 1. Attention to body mass index and early detection of obesity
- Regularly checking and monitoring a child’s height and weight are the first steps toward prevention. In Korea, there is a comprehensive infant health examination program conducted over seven stages from 4 to 71 months of age. Additionally, during the school-age years, a school health program involves annual measurement of height and weight, with referrals to medical institutions in cases of abnormalities.
- 2. Promoting healthy diet and physical activity
- Healthy eating habits should be promoted and harmful eating habits should be discouraged. Consuming fresh vegetables and fruits while reducing the intake of refined carbohydrates can help reduce caloric intake, thereby decreasing the risk of obesity [44]. It is recommended to limit the intake of sugar-sweetened beverages and consume whole fruits, which contain fiber that can provide a sense of fullness, rather than fruit juices [45,46]. Moreover, selecting low-energy-density foods, consuming a healthy breakfast daily, sharing meals with family, minimizing dining out, and educating oneself on portion sizes are essential strategies for maintaining appropriate meal sizes [47-50].
- Physical activity is a critical factor in preventing and managing obesity, and increasing the amount of activity and reducing inactive time are crucial [51]. Children and adolescents should engage in moderate-to-vigorous physical activity for at least 20 minutes per day (aiming for 60 minutes) at least five times per week, along with reduced caloric intake, to improve metabolism and reduce the likelihood of developing obesity [40]. Preschool children should engage in outdoor play and games, whereas school-aged children and adolescents should engage in structured physical activities, including exercises [48,52]. Prolonged screen time (e.g., on a television [TV], computer, or tablet) diminishes physical activity, heightens the likelihood of exposure to fast food advertising through the media, and may correlate with irregular sleep patterns. These factors are significantly associated with an increased risk of being overweight and obese [53-56]. It is advisable to curtail screen time to 1 to 2 hours daily and enhance physical activity. Furthermore, a TV should not be placed in the child’s sleeping area and watching TV during mealtime should be avoided [57].
- The association between breastfeeding and pediatric obesity has long been a matter of debate. A meta-analysis showed that breastfeeding is an essential factor in preventing obesity in children [58]. A longer breastfeeding duration was associated with a decrease in pediatric obesity [59]. In particular, when breastfeeding continued for more than 7 months, the risk of obesity significantly decreased [60].
- The risk of obesity doubles with shorter sleep duration [61]. Notably, sleep duration was inversely correlated with diet energy density and the consumption of sugar-sweetened beverages [62]. Irregular sleep patterns can adversely affect appetite and reduce insulin sensitivity [63]. Thus, reduced sleep duration is associated with the development of obesity, highlighting the importance of promoting healthy sleep patterns. Psychosocial stress and adverse childhood experiences are increasingly being identified as risk factors for obesity [42]. Maintaining emotional stability and managing stress can also improve dietary and lifestyle habits [64].
- 3. Creating a health-promoting environment
- Comprehensive behavioral interventions are required to prevent pediatric obesity. This requires the involvement of the family, school, and community surrounding the child.
- The home environment provides a crucial setting for shaping the lifestyle behaviors of children such as dietary habits, physical activity, and sleep patterns. Owing not only to genetic characteristics but also the shared obesogenic environment, a child’s BMI significantly correlates with the parents’ BMI [65]. Furthermore, the higher the parental BMI, the greater the pediatric obesity rate [66]. Participation by the entire family, rather than by individuals alone, is essential to ameliorate the obesogenic environment. Family-based lifestyle modifications, encompassing enhanced nutrition and physical activity, have demonstrated positive outcomes in managing the weight of children [67]. Notably, high parental involvement has been effective in preventing obesity and overweight in children [68].
- Schools serve as crucial environments in which children and adolescents spend a substantial portion of their time. Schools offer exceptional opportunities to deliver quality meals through school lunches and nutritional education, thereby playing a pivotal role in preventing obesity by fostering a healthy living environment. Furthermore, there are experts, such as teachers, counselors, health educators, and nutritionists, and facilities, such as classrooms, gyms, and playgrounds, that can be effectively utilized. Notably, education about healthy eating has been shown to decrease the consumption of unhealthy foods and sugary drinks [69]. Moreover, exercise interventions facilitated by physical activity programs in school settings have been shown to reduce the BMI of children [70]. School-based obesity-prevention programs significantly contribute to weight loss and are instrumental in promoting health by encouraging healthy eating habits and physical activity. Psychosocial support systems are needed to reduce stress and overcome adverse childhood experiences [42].
- Families and schools are community members that can influence the social environment. Ultimately, the environment for healthier choices should be improved through community-based obesity-prevention programs. Healthy foods and beverages should be incentivized, whereas harmful foods should be taxed to encourage accessibility to healthy options. By introducing a sugar tax and imposing a tax based on sugar content, companies were incentivized to reduce sugar content, and consumers were encouraged to reduce sugar-sweetened beverage consumption [71,72]. Additionally, restricting food advertising targeting children in mass media can limit the promotion of high-energy-density foods and beverages to children, who are easily influenced by TV commercials and similar platforms. Attaching nutritional labels to food products and regulating portion sizes can also help reduce caloric intake, thus lowering the incidence of pediatric obesity [73,74]. Enhancing the accessibility and economic viability of sports facilities, along with the expansion of public open spaces in urban centers, facilitates physical activity during leisure time [75].
- It is important that a diverse group of experts with a wealth of experience in pediatric obesity, such as healthcare professionals, nutritionists, psychologists, social workers, and exercise specialists, collaborate to coordinate community facilities and resources. Currently, national organizations such as the Ministry of Health and Welfare; Ministry of Education; Ministry of Culture, Sports, and Tourism; and Ministry of Food and Drug Safety are carrying out various projects and policies to prevent obesity in children and adolescents; however, these primarily focus on improving individual lifestyle modifications. In addition, some initiatives are implemented temporarily or provide overlapping support to the same targets; therefore, establishing effective policies through cooperation between institutions is important [76]. This will facilitate the development of a healthy community environment where nutritious food can be purchased affordably and conveniently and where opportunities for vigorous physical activity are available. Stress management and emotional support should be improved by increasing access to mental health services and strengthening education. These community-level strategies are crucial for the long-term prevention of pediatric obesity and require sustained focus.
Prevention of pediatric obesity
- The prevalence of obesity in children and adolescents has been increasing, leading to the development of comorbidities. This trend significantly increases the likelihood of obesity persisting into adulthood, thereby escalating the risk of metabolic syndrome and obesity-related complications. First, to solve the problem of pediatric obesity, it is necessary to understand its current status and trends. Obesity is a preventable disease. However, once it occurs, successful treatment becomes challenging, making its prevention crucial. To prevent obesity in children and adolescents, promoting healthy diet and physical activity through a multidisciplinary approach is important. Furthermore, cooperation and policy support from local communities, including families and schools, are essential. Effective prevention and active management of obesity in children and adolescents are crucial to ensure growth into healthy adults. Importantly, this would not only enhance individual health by increasing life expectancy and quality of life but also potentially diminish the socioeconomic costs associated with the transition of childhood and adolescent obesity into adult obesity, thereby benefiting the nation.
Conclusion
-
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
-
Funding
None.
Article information
Fig. 1.Prevalence of overweight and obesity among Korean children and adolescents aged 6 to 18 years from 2014 to 2022. NSHE, National School Health Examination; KNHANES, Korea National Health and Nutrition Examination Survey.


Table 1.Prevalence of overweight and obesity among Korean children and adolescents aged 6 to 18 years from 2014 to 2022 based on NSHE data
Table 2.Prevalence of overweight and obesity among Korean children and adolescents aged 6 to 18 years from 2017 to 2021 based on KNHANES data
Table 3.Obesity-prevention strategies for different age groups in children and adolescents
- 1. Lobstein T, Jackson-Leach R, Moodie ML, Hall KD, Gortmaker SL, Swinburn BA, et al. Child and adolescent obesity: part of a bigger picture. Lancet 2015;385:2510–20.ArticlePubMedPMC
- 2. Di Cesare M, Sorić M, Bovet P, Miranda JJ, Bhutta Z, Stevens GA, et al. The epidemiological burden of obesity in childhood: a worldwide epidemic requiring urgent action. BMC Med 2019;17:212.ArticlePubMedPMC
- 3. Schwartz MW, Seeley RJ, Zeltser LM, Drewnowski A, Ravussin E, Redman LM, et al. Obesity pathogenesis: an endocrine society scientific statement. Endocr Rev 2017;38:267–96.ArticlePubMedPMC
- 4. Grandone A, Di Sessa A, Umano GR, Toraldo R, Miraglia Del Giudice E. New treatment modalities for obesity. Best Pract Res Clin Endocrinol Metab 2018;32:535–49.ArticlePubMed
- 5. Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev 2008;9:474–88.ArticlePubMed
- 6. Simmonds M, Llewellyn A, Owen CG, Woolacott N. Predicting adult obesity from childhood obesity: a systematic review and meta-analysis. Obes Rev 2016;17:95–107.ArticlePubMed
- 7. Sonntag D. Why early prevention of childhood obesity is more than a medical concern: a health economic approach. Ann Nutr Metab 2017;70:175–8.ArticlePubMedPDF
- 8. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128•9 million children, adolescents, and adults. Lancet 2017;390:2627–42.ArticlePubMedPMC
- 9. World Health Organization (WHO). WHO fact sheet: Obesity and overweight [Internet]. Geneva: WHO; 2024 [cited 2024 Mar 29]. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
- 10. Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC. Prevalence of obesity and severe obesity in US children, 1999-2016. Pediatrics 2018;141:e20173459.ArticlePubMedPDF
- 11. Olds T, Maher C, Zumin S, Péneau S, Lioret S, Castetbon K, et al. Evidence that the prevalence of childhood overweight is plateauing: data from nine countries. Int J Pediatr Obes 2011;6:342–60.ArticlePubMed
- 12. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 2014;311:806–14.ArticlePubMedPMC
- 13. Skinner AC, Skelton JA. Prevalence and trends in obesity and severe obesity among children in the United States, 1999-2012. JAMA Pediatr 2014;168:561–6.ArticlePubMed
- 14. Kim DU, Rie KC. Studies on height, sitting height and relative sitting height of Korean primary school children in urban areas. J Korean Pediatr Soc 1967;10:585–98.
- 15. Moon HR, Yun DJ. Height and weight (and other measurements) of children in Korea 1975. J Korean Pediatr Soc 1978;21:183–97.
- 16. Shim TS, Ko KW. Physical growth of children in Korean, 1985. J Korean Pediatr Soc 1985;29:1–22.
- 17. Lee DH, Hong YM, Lee KY; The Committee for Public Health Statistics; The Committee for Nutrition. 1998 Korean National Growth Charts. Seoul: The Korean Pediatric Society; 1999.
- 18. Moon JS, Lee SY, Nam CM, Choi JM, Choe BK, Seo JW, et al. 2007 Korean National Growth Charts: review of developmental process and an outlook. Korean J Pediatr 2008;51:1–25.Article
- 19. Kim JH, Yun S, Hwang SS, Shim JO, Chae HW, Lee YJ, et al. The 2017 Korean National Growth Charts for children and adolescents: development, improvement, and prospects. Korean J Pediatr 2018;61:135–49.ArticlePubMedPMCPDF
- 20. Park YS, Lee DH, Choi JM, Kang YJ, Kim CH. Trend of obesity in school age children in Seoul over the past 23 years. Korean J Pediatr 2004;47:247–57.
- 21. Oh K, Jang MJ, Lee NY, Moon JS, Lee CG, Yoo MH, et al. Prevalence and trends in obesity among Korean children and adolescents in 1997 and 2005. Korean J Pediatr 2008;51:950–5.Article
- 22. Kim JH, Moon JS. Secular trends in pediatric overweight and obesity in Korea. J Obes Metab Syndr 2020;29:12–7.ArticlePubMedPMC
- 23. Nam HK, Kim HR, Rhie YJ, Lee KH. Trends in the prevalence of extreme obesity among Korean children and adolescents from 2001 to 2014. J Pediatr Endocrinol Metab 2017;30:517–23.ArticlePubMed
- 24. Choe J, Kim J, Moon JS. Cutoff values of body mass index for severe obesity in Korean children and adolescents: the 99th percentile versus 120% of the 95th percentile. Ann Pediatr Endocrinol Metab 2023;28:131–7.ArticlePubMedPMCPDF
- 25. Student Health Information Center, Ministry of Education. Student Health Information Center Website [Internet]. Cheongju, Korea: Student Health Information Center, Ministry of Education; 2024 [cited 2024 Mar 18]. https://schoolhealth.kr/index.do.
- 26. Korea Disease Control and Prevention Agency. The Korea National Health and Nutrition Examination Survey (KNHANES), 2010-2022 [Internet]. Cheongju: Korea Disease Control and Prevention Agency; 2024 [cited 2024 Mar 19]. https://knhanes.kdca.go.kr/knhanes/sub04/sub04_04_01.do.
- 27. Park HK, Seo JY, Jung HW, Lim JS. Prevalence and trends in obesity and severe obesity in Korean children and adolescents, 2007-2020: a population-based study. Pediatr Int 2023;65:e15472.ArticlePubMedPDF
- 28. Kang S, Seo MY, Kim SH, Park MJ. Changes in lifestyle and obesity during the COVID-19 pandemic in Korean adolescents: based on the Korea Youth Risk Behavior Survey 2019 and 2020. Ann Pediatr Endocrinol Metab 2022;27:281–8.ArticlePubMedPMCPDF
- 29. Abbasi A, Juszczyk D, van Jaarsveld CH, Gulliford MC. Body mass index and incident type 1 and type 2 diabetes in children and young adults: a retrospective cohort study. J Endocr Soc 2017;1:524–37.ArticlePubMedPMC
- 30. Kim HY, Kim JH. Temporal trends in the prevalence of metabolically healthy overweight and obesity in Korean youth: data from the Korea National Health and Nutrition Examination Survey 2011-2019. Ann Pediatr Endocrinol Metab 2022;27:134–41.ArticlePubMedPMCPDF
- 31. Vos MB, Abrams SH, Barlow SE, Caprio S, Daniels SR, Kohli R, et al. NASPGHAN clinical practice guideline for the diagnosis and treatment of nonalcoholic fatty liver disease in children: recommendations from the Expert Committee on NAFLD (ECON) and the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN). J Pediatr Gastroenterol Nutr 2017;64:319–34.ArticlePubMedPMC
- 32. Wühl E. Hypertension in childhood obesity. Acta Paediatr 2019;108:37–43.ArticlePubMedPDF
- 33. Calcaterra V, Klersy C, Muratori T, Telli S, Caramagna C, Scaglia F, et al. Prevalence of metabolic syndrome (MS) in children and adolescents with varying degrees of obesity. Clin Endocrinol (Oxf) 2008;68:868–72.ArticlePubMed
- 34. Chung YL, Rhie YJ. Severe Obesity in children and adolescents: metabolic effects, assessment, and treatment. J Obes Metab Syndr 2021;30:326–35.ArticlePubMedPMC
- 35. Kim M, Kim J. Cardiometabolic risk factors and metabolic syndrome based on severity of obesity in Korean children and adolescents: data from the Korea National Health and Nutrition Examination Survey 2007-2018. Ann Pediatr Endocrinol Metab 2022;27:289–99.ArticlePubMedPMCPDF
- 36. Li S, Chen W, Srinivasan SR, Bond MG, Tang R, Urbina EM, et al. Childhood cardiovascular risk factors and carotid vascular changes in adulthood: the Bogalusa Heart Study. JAMA 2003;290:2271–6.ArticlePubMed
- 37. Twig G, Yaniv G, Levine H, Leiba A, Goldberger N, Derazne E, et al. Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood. N Engl J Med 2016;374:2430–40.ArticlePubMed
- 38. Kim JH. Overview of pediatric obesity: diagnosis, epidemiology, and significance. J Korean Med Assoc 2021;64:401–9.ArticlePDF
- 39. Brown V, Ananthapavan J, Sonntag D, Tan EJ, Hayes A, Moodie M. The potential for long-term cost-effectiveness of obesity prevention interventions in the early years of life. Pediatr Obes 2019;14:e12517.ArticlePubMedPDF
- 40. Styne DM, Arslanian SA, Connor EL, Farooqi IS, Murad MH, Silverstein JH, et al. Pediatric obesity-assessment, treatment, and prevention: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 2017;102:709–57.ArticlePubMedPMCPDF
- 41. Masood B, Moorthy M. Causes of obesity: a review. Clin Med (Lond) 2023;23:284–91.ArticlePubMedPMC
- 42. Kyler KE, Hall M, Halvorson EE, Davis AM. Associations between obesity and adverse childhood experiences in the United States. Child Obes 2021;17:342–8.ArticlePubMed
- 43. Bleich SN, Segal J, Wu Y, Wilson R, Wang Y. Systematic review of community-based childhood obesity prevention studies. Pediatrics 2013;132:e201–10.ArticlePubMedPMCPDF
- 44. James J, Thomas P, Cavan D, Kerr D. Preventing childhood obesity by reducing consumption of carbonated drinks: cluster randomised controlled trial. BMJ 2004;328:1237.ArticlePubMedPMC
- 45. Dietz WH. Sugar-sweetened beverages, milk intake, and obesity in children and adolescents. J Pediatr 2006;148:152–4.ArticlePubMed
- 46. Shefferly A, Scharf RJ, DeBoer MD. Longitudinal evaluation of 100% fruit juice consumption on BMI status in 2-5-year-old children. Pediatr Obes 2016;11:221–7.ArticlePubMed
- 47. Epstein LH, Paluch RA, Beecher MD, Roemmich JN. Increasing healthy eating vs. reducing high energy-dense foods to treat pediatric obesity. Obesity (Silver Spring) 2008;16:318–26.ArticlePubMedPMCPDF
- 48. Kang E, Hong YH, Kim J, Chung S, Kim KK, Haam JH, et al. Obesity in children and adolescents: 2022 update of clinical practice guidelines for obesity by the Korean Society for the Study of Obesity. J Obes Metab Syndr 2024;33:11–9.ArticlePubMedPMC
- 49. Rolls BJ. Plenary lecture 1: dietary strategies for the prevention and treatment of obesity. Proc Nutr Soc 2010;69:70–9.ArticlePubMed
- 50. DiSantis KI, Birch LL, Davey A, Serrano EL, Zhang J, Bruton Y, et al. Plate size and children's appetite: effects of larger dishware on self-served portions and intake. Pediatrics 2013;131:e1451–8.ArticlePubMedPDF
- 51. Crespo CJ, Smit E, Troiano RP, Bartlett SJ, Macera CA, Andersen RE. Television watching, energy intake, and obesity in US children: results from the third National Health and Nutrition Examination Survey, 1988-1994. Arch Pediatr Adolesc Med 2001;155:360–5.ArticlePubMed
- 52. Erçelik ZE, Çağlar S. Effectiveness of active video games in overweight and obese adolescents: a systematic review and meta-analysis of randomized controlled trials. Ann Pediatr Endocrinol Metab 2022;27:98–104.ArticlePubMedPMCPDF
- 53. Andersen RE, Crespo CJ, Bartlett SJ, Cheskin LJ, Pratt M. Relationship of physical activity and television watching with body weight and level of fatness among children: results from the Third National Health and Nutrition Examination Survey. JAMA 1998;279:938–42.ArticlePubMed
- 54. Robinson TN, Banda JA, Hale L, Lu AS, Fleming-Milici F, Calvert SL, et al. Screen media exposure and obesity in children and adolescents. Pediatrics 2017;140(Suppl 2):S97–101.ArticlePubMedPMCPDF
- 55. LeBourgeois MK, Hale L, Chang AM, Akacem LD, Montgomery-Downs HE, Buxton OM. Digital media and sleep in childhood and adolescence. Pediatrics 2017;140(Suppl 2):S92–6.ArticlePubMedPDF
- 56. Fang K, Mu M, Liu K, He Y. Screen time and childhood overweight/obesity: a systematic review and meta-analysis. Child Care Health Dev 2019;45:744–53.ArticlePubMedPDF
- 57. Council on Communications and Media. Media and young minds. Pediatrics 2016;138:e20162591.ArticlePubMedPDF
- 58. Yan J, Liu L, Zhu Y, Huang G, Wang PP. The association between breastfeeding and childhood obesity: a meta-analysis. BMC Public Health 2014;14:1267.ArticlePubMedPMCPDF
- 59. Harder T, Bergmann R, Kallischnigg G, Plagemann A. Duration of breastfeeding and risk of overweight: a meta-analysis. Am J Epidemiol 2005;162:397–403.ArticlePubMed
- 60. Kramer MS, Matush L, Vanilovich I, Platt RW, Bogdanovich N, Sevkovskaya Z, et al. Effects of prolonged and exclusive breastfeeding on child height, weight, adiposity, and blood pressure at age 6.5 y: evidence from a large randomized trial. Am J Clin Nutr 2007;86:1717–21.ArticlePubMed
- 61. Fatima Y, Doi SA, Mamun AA. Longitudinal impact of sleep on overweight and obesity in children and adolescents: a systematic review and bias-adjusted meta-analysis. Obes Rev 2015;16:137–49.ArticlePubMed
- 62. Kjeldsen JS, Hjorth MF, Andersen R, Michaelsen KF, Tetens I, Astrup A, et al. Short sleep duration and large variability in sleep duration are independently associated with dietary risk factors for obesity in Danish school children. Int J Obes (Lond) 2014;38:32–9.ArticlePubMedPDF
- 63. Weng SF, Redsell SA, Swift JA, Yang M, Glazebrook CP. Systematic review and meta-analyses of risk factors for childhood overweight identifiable during infancy. Arch Dis Child 2012;97:1019–26.ArticlePubMed
- 64. Ahn SN, Zhang H, Berlin KS, Levy M, Kabra R. Adverse childhood experiences and childhood obesity: a path analysis approach. Child Health Care 2020;49:247–66.Article
- 65. Danielzik S, Langnäse K, Mast M, Spethmann C, Müller MJ. Impact of parental BMI on the manifestation of overweight 5-7 year old children. Eur J Nutr 2002;41:132–8.ArticlePubMedPDF
- 66. Whitaker KL, Jarvis MJ, Beeken RJ, Boniface D, Wardle J. Comparing maternal and paternal intergenerational transmission of obesity risk in a large population-based sample. Am J Clin Nutr 2010;91:1560–7.ArticlePubMed
- 67. Chai LK, Collins C, May C, Brain K, Wong See D, Burrows T. Effectiveness of family-based weight management interventions for children with overweight and obesity: an umbrella review. JBI Database System Rev Implement Rep 2019;17:1341–427.ArticlePubMed
- 68. van der Kruk JJ, Kortekaas F, Lucas C, Jager-Wittenaar H. Obesity: a systematic review on parental involvement in long-term European childhood weight control interventions with a nutritional focus. Obes Rev 2013;14:745–60.ArticlePubMedPMC
- 69. Ickovics JR, Duffany KO, Shebl FM, Peters SM, Read MA, Gilstad-Hayden KR, et al. Implementing school-based policies to prevent obesity: cluster randomized trial. Am J Prev Med 2019;56:e1–11.ArticlePubMedPMC
- 70. Mei H, Xiong Y, Xie S, Guo S, Li Y, Guo B, et al. The impact of long-term school-based physical activity interventions on body mass index of primary school children: a meta-analysis of randomized controlled trials. BMC Public Health 2016;16:205.ArticlePubMedPMC
- 71. Teng AM, Jones AC, Mizdrak A, Signal L, Genç M, Wilson N. Impact of sugar-sweetened beverage taxes on purchases and dietary intake: systematic review and meta-analysis. Obes Rev 2019;20:1187–204.ArticlePubMedPMCPDF
- 72. Goiana-da-Silva F, Severo M, Cruz E Silva D, Gregório MJ, Allen LN, Muc M, et al. Projected impact of the Portuguese sugar-sweetened beverage tax on obesity incidence across different age groups: a modelling study. PLoS Med 2020;17:e1003036.ArticlePubMedPMC
- 73. Anastasiou K, Miller M, Dickinson K. The relationship between food label use and dietary intake in adults: a systematic review. Appetite 2019;138:280–91.ArticlePubMed
- 74. Nielsen SJ, Popkin BM. Patterns and trends in food portion sizes, 1977-1998. JAMA 2003;289:450–3.ArticlePubMed
- 75. Díez J, Gullón P, Sandín Vázquez M, Álvarez B, Martín MD, Urtasun M, et al. A community-driven approach to generate urban policy recommendations for obesity prevention. Int J Environ Res Public Health 2018;15:635.ArticlePubMedPMC
- 76. Park SJ, Chung SC, Jeong HS, Noh YM, Kang EG, Hong YH. Policy suggestion on empowerment of prevention and management of pediatric obesity. Public Health Weekly Report 2024;17:840–58.Article
References
Figure & Data
References
Citations
Citations to this article as recorded by 

- Figure
- Related articles
-
- The pathophysiology of diabetic foot: a narrative review
- Management and rehabilitation of moderate-to-severe diabetic foot infection: a narrative review
- Management of diabetic foot ulcers: a narrative review
- Role of gene therapy in treatment of cancer with craniofacial regeneration—current molecular strategies, future perspectives, and challenges: a narrative review
- Advances in management of pediatric chronic immune thrombocytopenia: a narrative review

 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine PubReader
PubReader ePub Link
ePub Link Cite
Cite