PubMed Central, CAS, DOAJ, KCI

Articles
- Page Path
- HOME > J Yeungnam Med Sci > Volume 37(4); 2020 > Article
-
Communication
Yeungnam University type drive-through (YU-Thru) coronavirus disease 2019 (COVID-19) screening system: a rapid and safe screening system -
Wan Seok Seo1
 , Seong Ho Kim2, Si Youn Song3
, Seong Ho Kim2, Si Youn Song3 , Jian Hur4
, Jian Hur4 , Jun Lee5
, Jun Lee5 , Sunho Choi6
, Sunho Choi6 , Yoojung Lee7
, Yoojung Lee7 , Dai Seg Bai7
, Dai Seg Bai7
-
Yeungnam University Journal of Medicine 2020;37(4):349-355.
DOI: https://doi.org/10.12701/yujm.2020.00640
Published online: September 18, 2020
1Department of Psychiatry, Yeungnam University College of Medicine, Daegu, Korea
2Department of Neurosurgery, Yeungnam University College of Medicine, Daegu, Korea
3Department of Otorhinolaryngology-Head and Neck Surgery, Yeungnam University College of Medicine, Daegu, Korea
4Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea
5Department of Neurology, Yeungnam University College of Medicine, Daegu, Korea
6Department of General Affairs, Yeungnam University Medical Center, Daegu, Korea
7Department of Psychiatry, Yeungnam University Hospital, Daegu, Korea
- Corresponding author: Wan Seok Seo Department of Psychiatry, Yeungnam University College of Medicine, 170 Hyeonchung-ro, Nam-gu, Daegu 42415, Korea Tel: +82-53-620-3340 Fax: +82-53-629-0256 E-mail: sws3901@ynu.ac.kr
Copyright © 2020 Yeungnam University College of Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 10,137 Views
- 99 Download
- 3 Crossref
- Abstract
- Introduction
- Brief overview of the conventional screening system and its’ limitations
- Design and launch of the Yeungnam University type drive-through screening system
- The four steps of Yeungnam University type drive-through system with a detailed description of each step
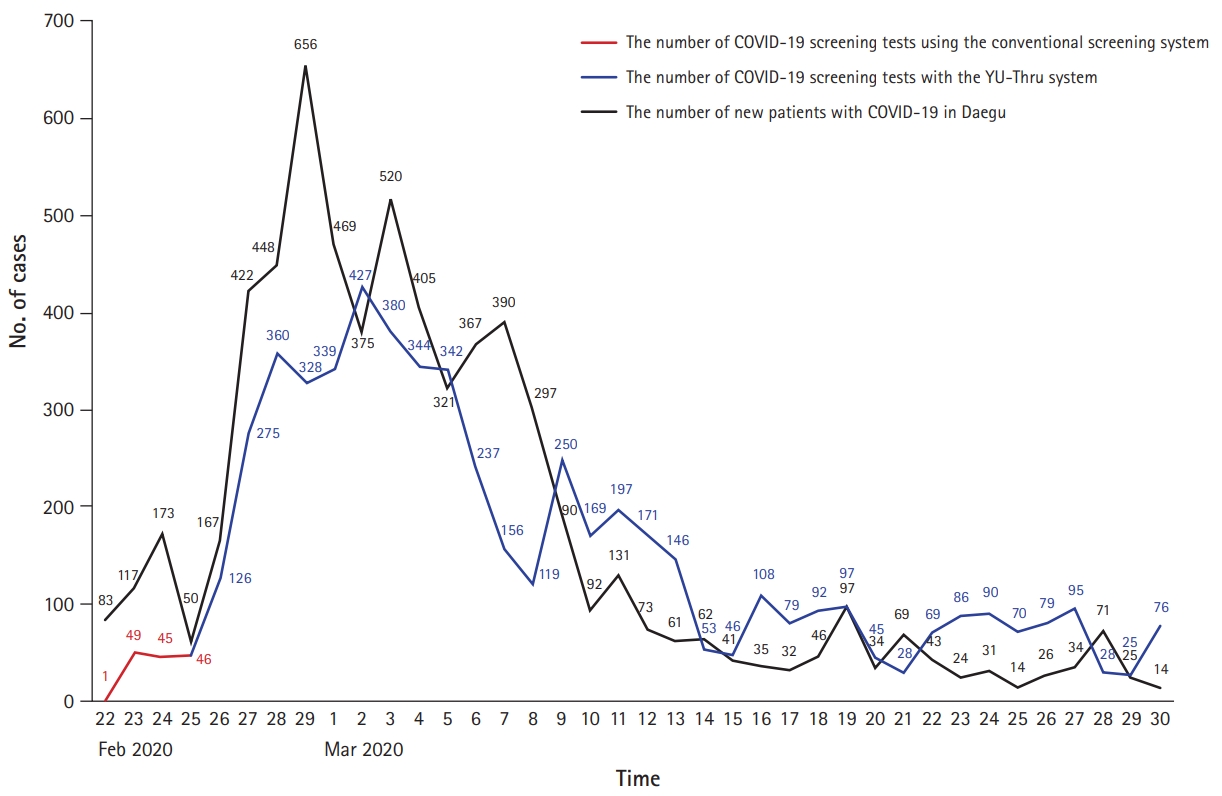
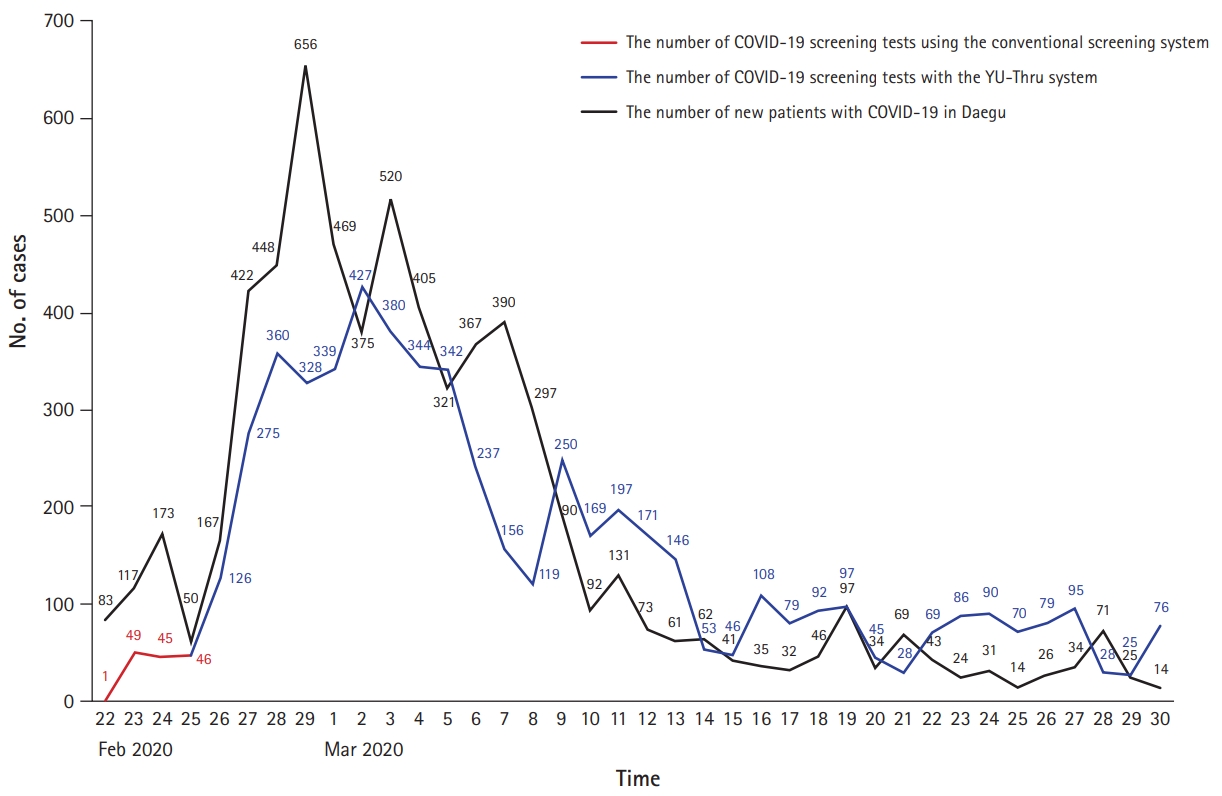
- Results and advantages of the Yeungnam University type drive-through screening system
- Limitations of the Yeungnam University type drive-through screening system and its’ specific concerns
- Conclusion
- Notes
- References
Figure & Data
References
Citations

- Experience of operating a medical humanities course at one medical school during the COVID-19: a retrospective study
Yu Ra Kim, Hye-won Shin, Young Hwan Lee, Seong-Yong Kim
Journal of Yeungnam Medical Science.2023; 40(2): 179. CrossRef - Lessons Learned From an Analysis of the Emergency Medical Services’ COVID-19 Drive-Through Testing Facilities in Israel
Itay Zmora, Evan Avraham Alpert, Uri Shacham, Nisim Mishraki, Eli Jaffe
Disaster Medicine and Public Health Preparedness.2022; 16(5): 2091. CrossRef - A study on the mental health of students at a medical school during COVID-19 outbreak: a retrospective study
Yu Ra Kim, Hye Jin Park, Bon-Hoon Koo, Ji Young Hwang, Young Hwan Lee
Journal of Yeungnam Medical Science.2022; 39(4): 314. CrossRef

 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine




 PubReader
PubReader ePub Link
ePub Link Cite
Cite