PubMed Central, CAS, DOAJ, KCI

Articles
- Page Path
- HOME > J Yeungnam Med Sci > Volume 39(1); 2022 > Article
-
Original article
Clinical investigation on acute pyelonephritis without pyuria: a retrospective observational study -
Hyung Keun Song
 , Dong Hyuk Shin
, Dong Hyuk Shin , Ji Ung Na
, Ji Ung Na , Sang Kuk Han
, Sang Kuk Han , Pil Cho Choi
, Pil Cho Choi , Jang Hee Lee
, Jang Hee Lee
-
Journal of Yeungnam Medical Science 2022;39(1):39-45.
DOI: https://doi.org/10.12701/yujm.2021.01207
Published online: August 11, 2021
Department of Emergency Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- Corresponding author: Jang Hee Lee, MD Department of Emergency Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, 29 Saemunan-ro, Jongno-gu, Seoul 03181, Korea Tel: +82-2-2001-3704 Fax: +82-2-2001-2891 E-mail: lemonpianote@gmail.com
Copyright © 2022 Yeungnam University College of Medicine, Yeungnam University Institute of Medical Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 6,779 Views
- 206 Download
Abstract
-
Background
- The current guidelines for the diagnosis of acute pyelonephritis (APN) recommend that APN be diagnosed based on the clinical features and the presence of pyuria. However, we observed that some of the patients who are diagnosed with APN do not have characteristic clinical features or pyuria at the initial examination. We performed this study to investigate the characteristics of APN without pyuria.
-
Methods
- A retrospective, cross-sectional study was conducted on 391 patients diagnosed with APN based on clinical and radiologic findings, between 2015 and 2019. The clinical features, laboratory results, and computed tomography (CT) findings were compared between patients with normal white blood cell (WBC) counts and those with abnormal WBC counts (WBC of 0–5/high power field [HPF] vs. >5/HPF) in urine.
-
Results
- More than 50% of patients with APN had no typical urinary tract symptoms and one-third of them had no costovertebral angle (CVA) tenderness. Eighty-eight patients (22.5%) had normal WBC counts (0–5/HPF) on urine microscopy. There was a negative correlation between pyuria (WBC of >5/HPF) and previous antibiotic use (odds ratio, 0.249; 95% confidence interval, 0.140–0.441; p<0.001), and the probability of pyuria was reduced by 75.1% in patients who took antibiotics before visiting the emergency room.
-
Conclusion
- The diagnosis of APN should not be overlooked even if there are no typical clinical features, or urine microscopic examination is normal. If a patient has already taken antibiotics at the time of diagnosis, imaging studies such as CT should be performed more actively, regardless of the urinalysis results.
- Acute pyelonephritis (APN) is characterized by upper urinary tract infection (UTI) symptoms (fever and flank pain) and pyuria [1,2]. However, symptoms related to upper UTI may be ambiguous, and sometimes only fever may appear [3,4]. If the symptoms presented by the patient are ambiguous or no symptoms other than fever are present, an objective test confirming the presence of pyuria is an important factor in the diagnosis of APN [5-7]. However, it is known that some patients diagnosed with APN do not have pyuria [8], which is frequently encountered in clinical practice.
- In this study, we investigated the number of white blood cells (WBC) observed in urine microscopy of female patients who were finally diagnosed with APN, to analyze how many patients with APN do not have pyuria, and to determine the differences in demographics, medical history, clinical features, physical examination findings, laboratory examination results, and abdominal computed tomography (CT) findings between APN with and without pyuria.
Introduction
- Ethical statements: This study was conducted as a retrospective, cross-sectional study after receiving approval from the Institutional Review Board (IRB) of Kangbuk Samsung Hospital (IRB No: 2020-11-030). The patient’s name, hospital number, date of birth, and social security number were deleted after assigning a serial number to each to maintain anonymity.
- 1. Subjects
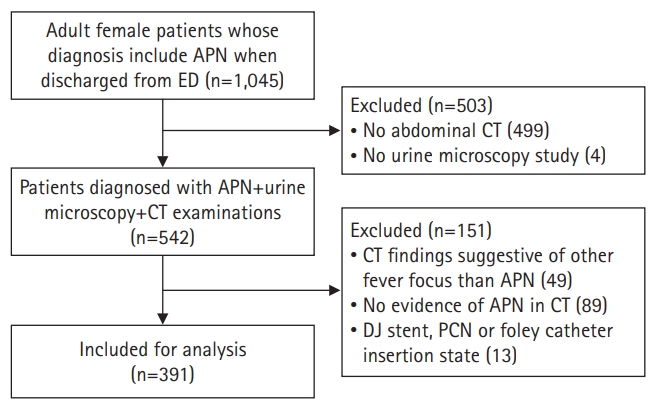
- In addition to the clinical diagnosis of APN, abdominal CT findings compatible with APN were also necessary to target only patients with a clear APN diagnosis. Female patients aged 18 years or older who visited our emergency department (ED) between January 2015 and December 2019 and whose final discharge diagnosis was APN were sought. Then, the CT findings were reviewed to exclude cases that did not have findings compatible with APN or had obvious causes of infection other than APN. In addition, patients who visited the hospital with a double J stent, percutaneous nephrostomy, and an indwelling foley catheter were also excluded (Fig. 1).
- 2. Outcome measures
- The urine WBC counts of the subjects determined by the microscopic study were arbitrarily classified into WBC 0–3/HPF, 4–5/HPF, 6–10/HPF, 11–20/HPF, and >20/HPF. We investigated the number of patients with APN having urine WBC counts in the normal range (0–5/HPF). After that, we compared the demographic characteristics, medical history, clinical features, physical examination findings, laboratory results, and CT findings between patients with normal WBC counts and those with abnormal WBC counts (0–5/HPF vs. >5/HPF). The patient’s age, underlying disease, past APN diagnosis experience, time from symptom onset to diagnosis, and antibiotic use prior to the ED visit were determined under demographic characteristics and medical history. It was not possible to determine the dose, duration, and type of antibiotics administered, and it was defined as “previous antibiotics use” if the patient took antibiotics even once before visiting the emergency room. The symptoms of upper UTI (fever and flank pain) and lower UTI (dysuria, frequency, urgency and residual urine sense) were recorded under clinical features. Costovertebral angle (CVA) tenderness was investigated for physical examination findings. WBC, neutrophil-to-lymphocyte ratio (NLR), C-reactive protein (CRP), procalcitonin, urine culture results, and blood culture results were investigated for laboratory findings. A positive urine culture test was defined as >105 colony-forming unit/mL. APN was defined as wedge-shaped low attenuation lesions from the renal medulla to the renal cortex and/or perinephric fat stranding on enhanced CT, and perinephric fat stranding on nonenhanced CT [9,10]. In addition, renal abscess formation and emphysematous change were considered APN. Those who had ureteritis or cystitis without APN were excluded from the study.
- 3. Statistical analysis
- Statistical analysis was performed using STATA (STATA 15.1, StataCorp LLC, College Station, TX, USA). Continuous variables are presented as mean and standard deviation, and categorical variables are described in terms of frequency (%). Continuous variables were compared using the Student t-test or Mann-Whitney U-test, while categorical variables were compared using the chi-square or Fisher exact test, according to the expected frequency. Statistical significance was set at p<0.05. Logistic regression was performed to confirm the correlation of major variables according to the amount of WBCs observed in the urine microscopic study. Multivariate logistic regression was performed using the variables considered to have an important effect on the presence of pyuria, with a p-value of 0.05 or less in univariate analysis.
Methods
- 1. General characteristics
- The average age of patients was 58.5 years, and the average time to visit the emergency room after symptom onset was 69.3 hours. Sixty-two patients (15.9%) had already taken antibiotics at least once before visiting the ED. More than 90% of patients with APN had a fever or a history of fever. Approximately 43.2% of patients had upper UTI symptoms (back pain or flank pain), and only 39.9% of patients had lower UTI symptoms (dysuria, frequency, urgency, and residual urine sense) at the time of ED visit. More than 50% of patients with APN did not have either upper or lower UTI symptoms. On physical examination, CVA tenderness was observed in 269 patients (68.8%), and approximately one-third of patients did not have CVA tenderness despite APN.
- A total of 223 patients underwent blood culture, and pathogens were identified in 80 patients (35.9%). Among the 138 patients who underwent urine culture, 99 (71.7%) had pathogenic bacteria.
- On abdominal CT, 89 patients did not have findings compatible with APN despite the clinical diagnosis of APN. There were 49 patients who had other causes of infection without APN findings on abdominal CT despite the clinical diagnosis of APN. Abscess formation or emphysematous changes were observed on abdominal CT in 24 patients (6.1%). There were 175 patients (44.8%) with ureteritis and 131 patients (33.5%) with cystitis (Table 1).
- 2. Comparison of patients with normal (0–5/HPF) and abnormal WBC count (>5/HPF) in urine microscopic study
- Eighty-eight patients (22.5%) had normal WBC counts (0–5/HPF) despite the clinical and CT diagnosis of APN, whereas 77.5% of patients had abnormal WBC counts (>5/HPF) on urine microscopic analysis (Table 2).
- When comparing APN with normal WBC (0–5/HPF) and with abnormal WBC (>5/HPF), there were no differences in age, underlying disease, duration from symptom onset to diagnosis, previous history of APN, upper UTI symptoms (fever and flank pain), lower UTI symptoms (dysuria, frequency, urgency, and residual urine sense), physical examination findings, blood WBC count, CRP, procalcitonin, and positive blood culture results. The variables that showed statistical differences were prior use of antibiotics, neutrophil percentage, NLR, and positive urine culture. Abscess formation or emphysematous changes in abdominal CT showed no difference, while ureteritis or cystitis showed a significant difference. Patients with APN accompanied by ureteritis or cystitis on CT showed a significantly higher prevalence of abnormal WBC counts (>5/HPF) on urine microscopic examination (Table 3).
- 3. Logistic regression analysis
- Table 4 shows the results of the univariate and multivariate logistic regression analyses. Among the variables with a p<0.05 in univariate analysis, previous antibiotic use, ureteritis, and cystitis were presumed to have an important effect on pyuria, and multivariate logistic regression analysis was performed using these variables. There was no multicollinearity between ureteritis and cystitis (phi coefficient=0.200). There was a strong and independent negative correlation between WBC of >5/HPF and previous antibiotic use at the time of diagnosis (odds ratio [OR]), 0.249; 95% confidence interval [CI], 0.140–0.441; p<0.001). If antibiotics were used at least once before visiting the emergency room, the chance of pyuria in urinalysis was reduced by 75.1%. None of the clinical signs or symptoms correlated with pyuria. Among the blood test results, neutrophil percentage and NLR showed a minimal positive correlation. For every one-unit increase in neutrophil percentage and NLR, the probability of pyuria was predicted to increase by 3.3% and 5.1%, respectively. The probability of pyuria was significantly higher in cases with ureteritis or cystitis on CT than in those without ureteritis or cystitis. In particular, in bilateral ureteritis, the OR for pyuria reached 9.7 (95% CI, 2.2–41.7; p=0.002) compared to cases without ureteritis.
Results
- This study showed that a relatively large proportion of patients with a confirmed diagnosis of APN based on clinical and radiological findings did not have typical clinical features and WBC counts on urine microscopic examination were within the normal range. Unlike the current guidelines for diagnosing APN based on clinical features and pyuria, this result suggests that it is difficult to exclude the diagnosis of APN based on clinical features and pyuria alone.
- Eighty-eight patients (22.5%) had normal WBC counts (0–5/HPF) on urine microscopic examination despite the clinical and CT diagnosis of APN. Among the several variables investigated, even a single use of antibiotics before visiting the ED was found to be highly correlated with normal urine WBC counts despite having APN. Therefore, prior use of antibiotics before ED visit should always be checked while taking a patient’s history for APN diagnosis. If the patient has already taken antibiotics, it is reasonable to diagnose APN based on the results of imaging tests such as CT rather than the results of urinalysis.
- On the other hand, the presence of abnormal WBC count showed a significant positive correlation with the presence of accompanying ureteritis or cystitis on CT. UTI is a retrograde ascending infection in which uropathogens arising from fecal flora, progress through the urethra and bladder to the ureter and kidney [11,12]. Clinical features appear in the form of urethritis and cystitis at the onset of UTI; hence, typical symptoms of lower UTI, such as dysuria, frequency, residual urine sense, and urgency are observed. However, as UTI progresses to ureteritis and pyelonephritis, upper UTI symptoms (fever and flank pain) appear. As lower UTI progresses to APN, the uropathogens may move from the lower urinary tract to the upper region of the tract; hence, bacteria and inflammation no longer remain in the lower urinary tract. However, in other cases, bacteria and inflammation may remain in the lower urinary tract. We assumed that if bacteria and inflammation remain in the lower urinary tract in patients with APN, cystitis should be observed along with APN findings on CT, and urine WBC count may be high.
- This study showed that more than half of patients with APN had neither upper UTI symptoms nor lower UTI symptoms, and approximately one-third of patients had no CVA tenderness. It is known that elderly patients with APN can only have a fever without typical symptoms of UTI [3,4]. However, in this study, the subjects were from a relatively younger age group with an average age of 58.5±18.7 years, which indicates that even in young female patients, typical upper UTI symptoms and lower UTI symptoms may not appear in APN. Physicians should always keep in mind that clinical features and physical examination may be ambiguous, and pyuria may not be present in patients with APN.
- The current APN diagnosis and treatment guidelines recommend that APN be diagnosed clinically based on the clinical features and the presence of pyuria, and to perform imaging studies only if the patient does not show clinical improvement after 72 hours of antibiotic treatment [1,2,13]. However, complicated APN requiring intervention or maintenance on a longer period of antibiotic treatment (kidney abscess, emphysematous change, ureter stone, etc.) is only identified after CT scans [8,14-16]. Moreover, as shown in the results of this study, there were many cases without APN findings or other infection sources than APN on CT, despite the clinical suspicion of APN. In this study, 16.4% of cases (89 of 542) had no evidence of APN on CT, and 9.0% of patients (49 of 542) with the clinical suspicion of APN had other sources of infection than APN on CT. For these reasons, the effectiveness of CT in APN diagnosis is gradually increasing. The authors recommend to actively perform CT on patients from their initial visit if APN cannot be ruled out, rather than insisting on the current guidelines that defer imaging studies.
- The main limitation of this study could be the selection bias. First, since this study was not intended for all patients with clinically suspected APN, but only for patients who had confirmed APN based on CT scan, there is a possibility that a selection bias could have occurred. Some patients may not have undergone CT because their symptoms, physical examination findings, and urine microscopy results were clearly suggestive of APN. These patients could have been included in the study if they had undergone CT. Second, this study included only patients who visited the ED; hence, patients who visited the outpatient clinic were excluded. Third, this was a single-center, retrospective study. Additionally, we have not studied whether there are differences in treatment and clinical prognosis between patients with and without pyuria.
- More than half of the patients with confirmed APN did not have typical symptoms or signs of UTI, and about one-quarter of the patients did not have pyuria. Usage of antibiotics before ED visit was strongly and independently correlated with normal WBC counts on urinalysis. The diagnosis of APN should not be overlooked even if there are no typical clinical features, or a urine microscopic analysis is normal. If no other cause of fever can be found and APN cannot be completely excluded, imaging tests such as CT should be more actively performed regardless of clinical features or presence of pyuria, especially if the patient has already taken antibiotics at the time of diagnosis.
Discussion
-
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
-
Author contributions
Conceptualization: all authors; Data curation, Investigation: HKS, JHL, DHS, JUN; Formal analysis: HKS, JHL, JUN, SKH, PCC; Supervision: DHS, JUN, SKH, PCC; Writing-original draft: HKS, JHL; Writing-review & editing: HKS, JHL, DHS, JUN, SKH, PCC.
Notes
| Degree of WBC | Data |
|---|---|
| 0–3/HPF | 46 (11.8) |
| 4–5/HPF | 42 (10.7) |
| 6–10/HPF | 61 (15.6) |
| 11–20/HPF | 68 (17.4) |
| >20/HPF | 174 (44.5) |
Values are presented as mean ± standard deviation or number (%).
WBC, white blood cell; HPF, high power field; APN, acute pyelonephritis; CVA, costovertebral angle; UTI, urinary tract infection; NLR, neutrophil-to-lymphocyte ratio; CRP, C-reactive protein; ESBL, extended-spectrum β-lactamase; CT, computed tomography.
| WBC of >5/HPF | OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value |
|---|---|---|---|---|
| Previous antibiotics use | 0.249 (0.140–0.441) | <0.001 | 0.249 (0.138–0.45)a) | <0.001 |
| Fever | 1.814 (0.816–4.035) | 0.144 | 1.916 (0.821–4.469)a) | 0.133 |
| Flank pain or back pain | 0.838 (0.520–1.351) | 0.469 | 1.033 (0.618–1.727)a) | 0.900 |
| Dysuria | 1.063 (0.647–1.745) | 0.809 | 1.089 (0.63–1.883)a) | 0.760 |
| Frequency | 1.240 (0.769–2.000) | 0.378 | 1.176 (0.7–1.976)a) | 0.539 |
| Residual urine sense | 0.785 (0.461–1.339) | 0.375 | 0.904 (0.507–1.611)a) | 0.731 |
| Urgency | 1.573 (0.851–2.907) | 0.149 | 1.513 (0.787–2.908)a) | 0.214 |
| CVA tenderness | 0.969 (0.580–1.620) | 0.905 | 1.105 (0.639–1.912)a) | 0.721 |
| WBC (×1,000/µL) | 1.05 (0.995–1.108) | 0.073 | 1.054 (0.996–1.115)a) | 0.068 |
| Neutrophil (%) | 1.038 (1.009–1.068) | 0.009 | 1.033 (1.003–1.065)a) | 0.030 |
| NLR | 1.059 (1.018–1.102) | 0.005 | 1.051 (1.009–1.094)a) | 0.017 |
| Lactate | 1.140 (0.659–1.973) | 0.639 | 1.04 (0.595–1.817)a) | 0.891 |
| CRP | 1.021 (0.992–1.051) | 0.164 | 1.014 (0.984–1.045)a) | 0.374 |
| Procalcitonin | 1.001 (0.977–1.025) | 0.960 | 1.001 (0.975–1.026)a) | 0.964 |
| Abscess formation or emphysematous change | 0.457 (0.193–1.084) | 0.075 | 0.511 (0.201–1.301)a) | 0.159 |
| Ureteritis | 2.157 (1.301–3.578) | 0.003 | 2.244 (1.328–3.789)b) | 0.003 |
| Unilateral ureteritis | 1.574 (0.928–2.672) | 0.093 | 1.645 (0.95–2.848)b) | 0.076 |
| Bilateral ureteritis | 9.445 (2.226–40.072) | 0.002 | 9.663 (2.239–41.698)b) | 0.002 |
| Cystitis | 2.519 (1.413–4.490) | 0.002 | 2.412 (1.334–4.36)b) | 0.004 |
- 1. Gupta K, Hooton TM, Naber KG, Wullt B, Colgan R, Miller LG, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis 2011;52:e103–20.ArticlePubMedPMC
- 2. Kang CI, Kim J, Park DW, Kim BN, Ha US, Lee SJ, et al. Clinical practice guidelines for the antibiotic treatment of community: acquired urinary tract infections. Infect Chemother 2018;50:67–100.ArticlePubMed
- 3. Matthews SJ, Lancaster JW. Urinary tract infections in the elderly population. Am J Geriatr Pharmacother 2011;9:286–309.ArticlePubMedPMC
- 4. Woodford HJ, George J. Diagnosis and management of urinary infections in older people. Clin Med (Lond) 2011;11:80–3.Article
- 5. Stamm WE. Measurement of pyuria and its relation to bacteriuria. Am J Med 1983;75(1B):53–8.PubMed
- 6. Colgan R, Williams M, Johnson JR. Diagnosis and treatment of acute pyelonephritis in women. Am Fam Physician 2011;84:519–26.Article
- 7. Pietrucha-Dilanchian P, Hooton TM. Diagnosis, treatment, and prevention of urinary tract infection. Microbiol Spectr 2016;4(6):10.1128/microbiolspec.UTI-0021-2015.ArticlePubMed
- 8. Rollino C, Beltrame G, Ferro M, Quattrocchio G, Sandrone M, Quarello F. Acute pyelonephritis in adults: a case series of 223 patients. Nephrol Dial Transplant 2012;27:3488–93.ArticlePubMed
- 9. Ifergan J, Pommier R, Brion MC, Glas L, Rocher L, Bellin MF. Imaging in upper urinary tract infections. Diagn Interv Imaging 2012;93:509–19.ArticlePubMedPMC
- 10. Lee A, Kim HC, Hwang SI, Chin HJ, Na KY, Chae DW, et al. Clinical usefulness of unenhanced computed tomography in patients with acute pyelonephritis. J Korean Med Sci 2018;33:e236.ArticlePubMedPMC
- 11. Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol 2015;13:269–84.ArticlePubMedPMC
- 12. McLellan LK, Hunstad DA. Urinary tract infection: pathogenesis and outlook. Trends Mol Med 2016;22:946–57.ArticlePubMed
- 13. Expert Panel on Urologic Imaging; Nikolaidis P, Dogra VS, Goldfarb S, Gore JL, Harvin HJ, et al. ACR Appropriateness Criteria® acute pyelonephritis. J Am Coll Radiol 2018;15(11 Suppl):S232–9.ArticlePubMed
- 14. Meng MV, Mario LA, McAninch JW. Current treatment and outcomes of perinephric abscesses. J Urol 2002;168(4 Pt 1):1337–40.ArticlePubMed
- 15. Aboumarzouk OM, Hughes O, Narahari K, Coulthard R, Kynaston H, Chlosta P, et al. Emphysematous pyelonephritis: time for a management plan with an evidence-based approach. Arab J Urol 2014;12:106–15.ArticlePubMed
- 16. Ramsey S, Robertson A, Ablett MJ, Meddings RN, Hollins GW, Little B. Evidence-based drainage of infected hydronephrosis secondary to ureteric calculi. J Endourol 2010;24:185–9.ArticlePubMed
References
Figure & Data
References
Citations

- Figure
- Related articles
-
- Optimal examination for traumatic nerve/muscle injuries in earthquake survivors: a retrospective observational study
- Impact of COVID-19 on the development of major mental disorders in patients visiting a university hospital: a retrospective observational study
- Association of advanced chronic kidney disease with diabetic retinopathy severity in older patients with diabetes: a retrospective cross-sectional study
- Incidence of congenital hypothyroidism by gestational age: a retrospective observational study

 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine PubReader
PubReader ePub Link
ePub Link Cite
Cite


