Indexed in: ESCI, Scopus, PubMed,
PubMed Central, CAS, DOAJ, KCI
PubMed Central, CAS, DOAJ, KCI
FREE article processing charge

Previous issues
- Page Path
- HOME > Browse Articles > Previous issues
Imagery
- "Wiyangmot Reservoir in Miryang, Korea"
- J Yeungnam Med Sci. 2022;39(3):i. Published online March 16, 2022
- DOI: https://doi.org/10.12701/jyms.2022.00171

- 2,294 View
- 68 Download
Editorial
- The blind spot and challenges in pain management
- Min Cheol Chang
- J Yeungnam Med Sci. 2022;39(3):179-180. Published online June 9, 2022
- DOI: https://doi.org/10.12701/jyms.2022.00339

- 2,224 View
- 62 Download
- 3 Web of Science
- 3 Crossref
-
 PDF
PDF -
Citations
Citations to this article as recorded by- Deep-Learning Algorithms for Prescribing Insoles to Patients with Foot Pain
Jeoung Kun Kim, Yoo Jin Choo, In Sik Park, Jin-Woo Choi, Donghwi Park, Min Cheol Chang
Applied Sciences.2023; 13(4): 2208. CrossRef - Effectiveness of transcranial alternating current stimulation for controlling chronic pain: a systematic review
Min Cheol Chang, Marie-Michèle Briand, Mathieu Boudier-Revéret, Seoyon Yang
Frontiers in Neurology.2023;[Epub] CrossRef - Use of QR Codes for Promoting a Home-Based Therapeutic Exercise in Patients with Lumbar Disc Herniation and Lumbar Spinal Stenosis: A Prospective Randomized Study
Min Cheol Chang, Donghwi Park, Yoo Jin Choo
Journal of Pain Research.2022; Volume 15: 4065. CrossRef
- Deep-Learning Algorithms for Prescribing Insoles to Patients with Foot Pain
Focused Review articles
- Pain in amyotrophic lateral sclerosis: a narrative review
- Soyoung Kwak
- J Yeungnam Med Sci. 2022;39(3):181-189. Published online June 8, 2022
- DOI: https://doi.org/10.12701/jyms.2022.00332

- 5,079 View
- 140 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF - Amyotrophic lateral sclerosis (ALS) is a rapidly progressive neurodegenerative condition characterized by loss of motor neurons, resulting in motor weakness of the limbs and/or bulbar muscles. Pain is a prevalent but neglected symptom of ALS, and it has a significant negative impact on the quality of life of patients and their caregivers. This review outlines the epidemiology, clinical characteristics, underlying mechanisms, and management strategies of pain in ALS to improve clinical practice and patient outcomes related to pain. Pain is a prevalent symptom among patients with ALS, with a variable reported prevalence. It may occur at any stage of the disease and can involve any part of the body without a specific pattern. Primary pain includes neuropathic pain and pain from spasticity or cramps, while secondary pain is mainly nociceptive, occurring with the progression of muscle weakness and atrophy, prolonged immobility causing degenerative changes in joints and connective tissue, and long-term home mechanical ventilation. Prior to treatment, the exact patterns and causes of pain must first be identified, and the treatment should be tailored to each patient. Treatment options can be classified into pharmacological treatments, including nonsteroidal anti-inflammatory drugs, antiepileptic drugs, drugs for cramps or spasticity, and opioid; and nonpharmacological treatments, including positioning, splints, joint injections, and physical therapy. The development of standardized and specific assessment tools for pain-specific to ALS is required, as are further studies on treatments to reduce pain, diminish suffering, and improve the quality of life of patients with ALS.
-
Citations
Citations to this article as recorded by- Health-related quality of life across disease stages in patients with amyotrophic lateral sclerosis: results from a real-world survey
Katie Stenson, T. E. Fecteau, L. O’Callaghan, P. Bryden, J. Mellor, J. Wright, L. Earl, O. Thomas, H. Iqbal, S. Barlow, S. Parvanta
Journal of Neurology.2024; 271(5): 2390. CrossRef - Amyotrophic Lateral Sclerosis and Pain: A Narrative Review from Pain Assessment to Therapy
Vincenzo Pota, Pasquale Sansone, Sara De Sarno, Caterina Aurilio, Francesco Coppolino, Manlio Barbarisi, Francesco Barbato, Marco Fiore, Gianluigi Cosenza, Maria Beatrice Passavanti, Maria Caterina Pace, Enzo Emanuele
Behavioural Neurology.2024; 2024: 1. CrossRef - Non-motor symptoms in patients with amyotrophic lateral sclerosis: current state and future directions
Bogdan Bjelica, Maj-Britt Bartels, Jasper Hesebeck-Brinckmann, Susanne Petri
Journal of Neurology.2024; 271(7): 3953. CrossRef - Likely Pathogenic Variants of Cav1.3 and Nav1.1 Encoding Genes in Amyotrophic Lateral Sclerosis Could Elucidate the Dysregulated Pain Pathways
Zsófia Flóra Nagy, Balázs Sonkodi, Margit Pál, Péter Klivényi, Márta Széll
Biomedicines.2023; 11(3): 933. CrossRef - Palliative Care in Amyotrophic Lateral Sclerosis
Sebastiano Mercadante, Lou'i Al-Husinat
Journal of Pain and Symptom Management.2023; 66(4): e485. CrossRef - The blind spot and challenges in pain management
Min Cheol Chang
Journal of Yeungnam Medical Science.2022; 39(3): 179. CrossRef - Synucleinopathy in Amyotrophic Lateral Sclerosis: A Potential Avenue for Antisense Therapeutics?
Bradley Roberts, Frances Theunissen, Francis L. Mastaglia, P. Anthony Akkari, Loren L. Flynn
International Journal of Molecular Sciences.2022; 23(16): 9364. CrossRef - Herbal medicine and acupuncture relieved progressive bulbar palsy for more than 3 years: A case report
Siyang Peng, Weiqian Chang, Yukun Tian, Yajing Yang, Shaohong Li, Jinxia Ni, Wenzeng Zhu
Medicine.2022; 101(45): e31446. CrossRef
- Health-related quality of life across disease stages in patients with amyotrophic lateral sclerosis: results from a real-world survey
- Ultrasound-guided interventions for controlling the thoracic spine and chest wall pain: a narrative review
- Donghwi Park, Min Cheol Chang
- J Yeungnam Med Sci. 2022;39(3):190-199. Published online April 26, 2022
- DOI: https://doi.org/10.12701/jyms.2022.00192

- 4,572 View
- 175 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Ultrasound-guided injection is useful for managing thoracic spine and chest wall pain. With ultrasound, pain physicians perform the injection with real-time viewing of major structures, such as the pleura, vasculature, and nerves. Therefore, the ultrasound-guided injection procedure not only prevents procedure-related adverse events but also increases the accuracy of the procedure. Here, ultrasound-guided interventions that could be applied for thoracic spine and chest wall pain were described. We presented ultrasound-guided thoracic facet joint and costotransverse joint injections and thoracic paravertebral, intercostal nerve, erector spinae plane, and pectoralis and serratus plane blocks. The indication, anatomy, Sonoanatomy, and technique for each procedure were also described. We believe that our article is helpful for clinicians to conduct ultrasound-guided injections for controlling thoracic spine and chest wall pain precisely and safely.
-
Citations
Citations to this article as recorded by- The blind spot and challenges in pain management
Min Cheol Chang
Journal of Yeungnam Medical Science.2022; 39(3): 179. CrossRef
- The blind spot and challenges in pain management
- The mechanism of action of pulsed radiofrequency in reducing pain: a narrative review
- Donghwi Park, Min Cheol Chang
- J Yeungnam Med Sci. 2022;39(3):200-205. Published online April 7, 2022
- DOI: https://doi.org/10.12701/jyms.2022.00101

- 5,043 View
- 137 Download
- 12 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF - Pain from nervous or musculoskeletal disorders is one of the most common complaints in clinical practice. Corticosteroids have a high pain-reducing effect, and their injection is generally used to control various types of pain. However, they have various adverse effects including flushing, hyperglycemia, allergic reactions, menstrual changes, immunosuppression, and adrenal suppression. Pulsed radiofrequency (PRF) is known to have a pain-reducing effect similar to that of corticosteroid injection, with nearly no major side effects. Therefore, it has been widely used to treat various types of pain, such as neuropathic, joint, discogenic, and muscle pain. In the current review, we outlined the pain-reducing mechanisms of PRF by reviewing previous studies. When PRF was first introduced, it was supposed to reduce pain by long-term depression of pain signaling from the peripheral nerve to the central nervous system. In addition, deactivation of microglia at the level of the spinal dorsal horn, reduction of proinflammatory cytokines, increased endogenous opioid precursor messenger ribonucleic acid, enhancement of noradrenergic and serotonergic descending pain inhibitory pathways, suppression of excitation of C-afferent fibers, and microscopic damage of nociceptive C- and A-delta fibers have been found to contribute to pain reduction after PRF application. However, the pain-reducing mechanism of PRF has not been clearly and definitely elucidated. Further studies are warranted to clarify the pain-reducing mechanism of PRF.
-
Citations
Citations to this article as recorded by- Pulsed Radiofrequency for Auriculotemporal Neuralgia: A Case Report
Yan Tereshko, Enrico Belgrado, Christian Lettieri, Simone Dal Bello, Giovanni Merlino, Gian Luigi Gigli, Mariarosaria Valente
Neurology International.2024; 16(2): 349. CrossRef - Transforaminal pulsed radiofrequency and epidural steroid injection on chronic lumbar radiculopathy: A prospective observational study from a tertiary care hospital in Vietnam
Viet-Thang Le, Phuoc Trong Do, Vu Duc Nguyen, Luan Trung Nguyen Dao, Ipek Saadet Edipoglu
PLOS ONE.2024; 19(4): e0292042. CrossRef - Pulsed Radiofrequency Ablation for Refractory Cancer-Related Leg Pain: A Case Report
Praveen Reddy Elmati, Tyler J Wilkinson, Alexander Bautista
Cureus.2024;[Epub] CrossRef - Anatomo-physiological basis and applied techniques of electrical neuromodulation in chronic pain
Giusy Guzzi, Attilio Della Torre, Andrea Bruni, Angelo Lavano, Vincenzo Bosco, Eugenio Garofalo, Domenico La Torre, Federico Longhini
Journal of Anesthesia, Analgesia and Critical Care.2024;[Epub] CrossRef - Radiofrecuencia del nervio supraescapular como estrategia analgésica para el dolor crónico de hombro. Revisión sistemática y metaanálisis
J. Sebastián Infante, N. Blackburn, J. Felipe Vargas
Revista Española de Anestesiología y Reanimación.2024;[Epub] CrossRef - Effect of pulsed radiofrequency to the suprascapular nerve (SSN) in treating frozen shoulder pain: A randomised controlled trial
Ghada Mohammad Abo Elfadl, Ayman Mamdouh Osman, Yasmeen Alaa-Eldeen Elmasry, Sherif Sayed Abdelraheem, Manal Hassanien
Journal of Perioperative Practice.2024;[Epub] CrossRef - Radiofrequency of suprascapular nerve as an analgesic strategy for chronic pain management. Systematic review and meta-analysis
J. Sebastián Infante, N. Blackburn, J. Felipe Vargas
Revista Española de Anestesiología y Reanimación (English Edition).2024;[Epub] CrossRef - Comparison of two distinct needle tip positions in pulsed radiofrequency for herpes zoster‐related pain
Shao‐jun Li, Dan Feng
CNS Neuroscience & Therapeutics.2023; 29(7): 1881. CrossRef - Previous Lumbar Spine Surgery Decreases the Therapeutic Efficacy of Dorsal Root Ganglion Pulsed Radiofrequency in Patients with Chronic Lumbosacral Radicular Pain
Jiri Jandura, Milan Vajda, Roman Kostysyn, Jiri Vanasek, Eva Cermakova, Jan Zizka, Pavel Ryska
Journal of Personalized Medicine.2023; 13(7): 1054. CrossRef - Spinal Injections: A Narrative Review from a Surgeon’s Perspective
Dong Ah Shin, Yoo Jin Choo, Min Cheol Chang
Healthcare.2023; 11(16): 2355. CrossRef - A narrative review of pulsed radiofrequency for the treatment of carpal tunnel syndrome
Himanshu Gupta, Colm Vance, Vishal Bansal, Ahilraj Siva
Pain Practice.2023;[Epub] CrossRef - Pulsed Radiofrequency 2 Hz Preserves the Dorsal Root Ganglion Neuron Physiological Ca2+ Influx, Cytosolic ATP Level, Δψm, and pERK Compared to 4 Hz: An Insight on the Safety of Pulsed Radiofrequency in Pain Management
Ristiawan Muji Laksono, Taufiq Agus Siswagama, Fa'urinda Riam Prabu Nery, Walter van der Weegen, Willy Halim
Journal of Pain Research.2023; Volume 16: 3643. CrossRef - Summary of the 48th KORSIS Symposium in 2023
Min Cheol Chang
International journal of Pain.2023; 14(2): 96. CrossRef - The blind spot and challenges in pain management
Min Cheol Chang
Journal of Yeungnam Medical Science.2022; 39(3): 179. CrossRef - Use of QR Codes for Promoting a Home-Based Therapeutic Exercise in Patients with Lumbar Disc Herniation and Lumbar Spinal Stenosis: A Prospective Randomized Study
Min Cheol Chang, Donghwi Park, Yoo Jin Choo
Journal of Pain Research.2022; Volume 15: 4065. CrossRef
- Pulsed Radiofrequency for Auriculotemporal Neuralgia: A Case Report
- The use of platelet-rich plasma in management of musculoskeletal pain: a narrative review
- Aung Chan Thu
- J Yeungnam Med Sci. 2022;39(3):206-215. Published online June 8, 2022
- DOI: https://doi.org/10.12701/jyms.2022.00290

- 4,892 View
- 137 Download
- 6 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF - Musculoskeletal pain is the most common pain reported by patients. Platelet-rich plasma (PRP) is widely used to treat musculoskeletal pain. However, the efficacy of PRP to treat this pain remains controversial. This review highlights the application of PRP in the treatment of musculoskeletal pain. PRP treatment appears to reduce pain and improve function in patients with musculoskeletal pain. However, there are limitations to the currently published studies. These limitations include the PRP preparation methods, type of activators, types of pathology to be treated, methods and times of administration, and association of PRP with other treatments.
-
Citations
Citations to this article as recorded by- Restraint stress-associated gastrointestinal injury and implications from the Evans blue-fed restraint stress mouse model
Der-Shan Sun, Te-Sheng Lien, Hsin-Hou Chang
Tzu Chi Medical Journal.2024; 36(1): 23. CrossRef - Injections of Platelet-Rich Plasma: An Emerging Novel Biological Cure for Low Back Pain?
Adarsh Jayasoorya , Nitin Samal, Gajanan Pisulkar, Kaustav Datta, Kevin Kawde
Cureus.2024;[Epub] CrossRef - Platelet-Rich Plasma in the Management of Temporomandibular Joint Pain in Young Adults With Temporomandibular Disorder
Santosh Kumar Mathpati, Gourav Jain, Vijay Mishra, Atul K Singh, Rahul Mishra, Bipin K Yadav
Cureus.2024;[Epub] CrossRef - Potentials and impact of platelet-rich plasma (PRP) on the regenerative properties of muscle tissue
V. H. Dzhyvak, I. M. Klishch, O. I. Khlibovska, S. S. Levenets
Biopolymers and Cell.2024; 40(1): 3. CrossRef - Injectable Lyophilized Chitosan-Thrombin-Platelet-Rich Plasma (CS-FIIa-PRP) Implant to Promote Tissue Regeneration: In Vitro and Ex Vivo Solidification Properties
Fiona Milano, Anik Chevrier, Gregory De Crescenzo, Marc Lavertu
Polymers.2023; 15(13): 2919. CrossRef - Systematic Review of Platelet-Rich Plasma for Low Back Pain
Edilson Silva Machado, Fabiano Pasqualotto Soares, Ernani Vianna de Abreu, Taís Amara da Costa de Souza, Robert Meves, Hans Grohs, Mary A. Ambach, Annu Navani, Renato Bevillaqua de Castro, Daniel Humberto Pozza, José Manuel Peixoto Caldas
Biomedicines.2023; 11(9): 2404. CrossRef - Potential Mechanism of Platelet-rich Plasma Treatment on Testicular Problems Related to Diabetes Mellitus
Rista Dwi Hermilasari, Dicky Moch Rizal, Yohanes Widodo Wirohadidjojo
Prague Medical Report.2023; 124(4): 344. CrossRef - The blind spot and challenges in pain management
Min Cheol Chang
Journal of Yeungnam Medical Science.2022; 39(3): 179. CrossRef
- Restraint stress-associated gastrointestinal injury and implications from the Evans blue-fed restraint stress mouse model
Original articles
- A comparative study of the psychological impacts of tasks related and unrelated to COVID-19 on nurses: a cross-sectional study
- Hyun Ji Kim, Geon Ho Lee
- J Yeungnam Med Sci. 2022;39(3):216-222. Published online November 3, 2021
- DOI: https://doi.org/10.12701/yujm.2021.01361

- 3,970 View
- 100 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
This study assessed the psychological impact of the outbreak of coronavirus disease 2019 (COVID-19) on university hospital nurses. It provides an assessment of mental health issues, including depression, anxiety, distress, and burnout of nurses dealing directly and indirectly with COVID-19.
Methods
In a web-based, cross-sectional study, 111 nurses from Daegu Catholic University Hospital in Korea were enrolled from August 4 to August 9, 2020. Patient Health Questionnaire-9, Generalized Anxiety Disorder-7, Impact of Event Scale-Revised, and Maslach Burnout Inventory were used to assess the psychological symptoms of depression, anxiety, psychological distress, and burnout among the study participants.
Results
Of 111 nurses, 35 (31.5%), nine (8.1%), 26 (23.4%), and 49 (44.1%) experienced depression, anxiety, distress, and burnout, respectively. Nurses who performed COVID-19–related tasks were more likely to have moderate depression (related vs. unrelated, 52.0% vs. 25.6%; p=0.037). There were no differences in anxiety, distress, and burnout between nurses with and without COVID-19–related tasks. More than 50% of the participants showed receptive and positive attitudes toward caring for COVID-19 patients.
Conclusion
Nurses who performed COVID-19–related tasks had a higher risk of depression. There were no significant differences in anxiety, distress, and burnout between the two groups. Since nurses who perform COVID-19–related tasks are more prone to psychological distress, continued psychiatric interventions are required for infectious disease outbreaks with a high mortality rate for healthcare workers who are emotionally vulnerable. -
Citations
Citations to this article as recorded by- Key predictors of psychological distress and wellbeing in Australian frontline healthcare workers during COVID-19 (Omicron wave)
Brian En Chyi Lee, Mathew Ling, Leanne Boyd, Craig A. Olsson, Jade Sheen
Frontiers in Psychology.2023;[Epub] CrossRef - Depression and burnout among Chinese nurses during COVID-19 pandemic: a mediation and moderation analysis model among frontline nurses and nonfrontline nurses caring for COVID-19 patients
Jingjun Wang, Xia Huang, Mengmeng Wang, Lei Huang, Ya Wang
BMC Psychiatry.2023;[Epub] CrossRef - Frontline nurses' burnout and its associated factors during the COVID-19 pandemic in South Korea
Eun-Young Noh, Yeon-Hwan Park, Young Jun Chai, Hyun Jeong Kim, Eunjin Kim
Applied Nursing Research.2022; 67: 151622. CrossRef - Characteristics of Occupational Burnout among Nurses of Various Specialties and in the Time of the COVID-19 Pandemic—Review
Robert Ślusarz, Klaudia Cwiekala-Lewis, Mariusz Wysokiński, Karolina Filipska-Blejder, Wiesław Fidecki, Monika Biercewicz
International Journal of Environmental Research and Public Health.2022; 19(21): 13775. CrossRef
- Key predictors of psychological distress and wellbeing in Australian frontline healthcare workers during COVID-19 (Omicron wave)
- Infection prevention measures and outcomes for surgical patients during a COVID-19 outbreak in a tertiary hospital in Daegu, South Korea: a retrospective observational study
- Kyung-Hwa Kwak, Jay Kyoung Kim, Ki Tae Kwon, Jinseok Yeo
- J Yeungnam Med Sci. 2022;39(3):223-229. Published online November 5, 2021
- DOI: https://doi.org/10.12701/yujm.2021.01431

- 5,263 View
- 95 Download
-
 Abstract
Abstract
 PDF
PDF - Background
The first large coronavirus disease 2019 (COVID-19) outbreak outside China occurred in Daegu. In response, we developed infection prevention measures for surgical patients during the outbreak at our hospital and retrospectively reviewed the outcomes of COVID-19–related surgical patients.
Methods
We reviewed the medical records of 118 COVID-19–related surgical patients and monitored their clinical outcomes until March 31, 2021. We also interviewed healthcare workers who participated in their perioperative care at Kyungpook National University Chilgok Hospital. The perioperative management guidelines for COVID-19–related patients were prepared through multidisciplinary discussions, including the infection control department, surgical departments, and anesthesiology department before and during the COVID-19 outbreak.
Results
One standard operating room was temporarily converted to a negative-pressure room by increasing the exhaust air volume, creating a relative pressure of −11.3 Pa. The healthcare workers were equipped with personal protective equipment according to the patient's classification of the risk of COVID-19 transmission. The 118 COVID-19–related patients underwent emergent surgery in the negative-pressure room, including three COVID-19–confirmed patients and five COVID-19–exposed patients.
Conclusion
All surgeries of the COVID-19–related patients were performed without specific adverse events or perioperative COVID-19 transmission. Our experience setting up a negative-pressure operating room and conservative perioperative protocol to prevent COVID-19 transmission will help plan and execute infection control measures in the future.
- Assessment of normal anal sphincter anatomy using transanal ultrasonography in healthy Korean volunteers: a retrospective observational study
- Daeho Shon, Sohyun Kim, Sung Il Kang
- J Yeungnam Med Sci. 2022;39(3):230-234. Published online December 2, 2021
- DOI: https://doi.org/10.12701/yujm.2021.01515

- 4,463 View
- 65 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
To date, there have been no studies on the normal anatomic values of the anal sphincter in healthy Koreans. Therefore, this study aimed to determine the normal anatomic values of transanal ultrasonography (TAUS).
Methods
The thickness of the external anal sphincter (EAS) and internal anal sphincter (IAS) was measured by TAUS from healthy Korean volunteers between September 2019 and August 2021.
Results
Thirty-six volunteers with a median age of 37 years (range, 20–77 years) and a median body mass index (BMI) of 23.5 kg/m2 (range, 17.2–31.2 kg/m2) were examined. The median thickness of the EAS at 4 cm and 2 cm from the anal verge was 7.4 mm (range, 5.8–8.8 mm) and 6.5 mm (range, 5.6–8.0 mm), respectively. The median thickness of the IAS at 2 cm from the anal verge was 1.8 mm (range, 0.8-4.3 mm). There were no differences in sphincter muscle thickness between the sexes. However, the EAS tended to thicken as the BMI increased (EAS at 2 cm and 4 cm from the anal verge, Spearman rho=0.433, 0.363; p=0.008 and p=0.029, respectively).
Conclusion
In healthy Korean, the median thickness of the IAS at 2 cm from the anal verge was 1.8 mm and the median thickness of the EAS at 2 cm and 4 cm from the anal verge was 6.5 mm and 7.4 mm respectively. There were no differences in anal sphincter thickness between sexes, but BMI was related to EAS thickness. -
Citations
Citations to this article as recorded by- Anal Sphincter Defect and Fecal Incontinence
Sherief Mansi, Karla Vaz, Neha R. Santucci, Khalil El-Chammas, Kahleb Graham, Nelson G. Rosen, Ajay Kaul
JPGN Reports.2022; 3(4): e254. CrossRef
- Anal Sphincter Defect and Fecal Incontinence
- Preemptive pyloroplasty for iatrogenic vagus nerve injury in intrahepatic cholangiocarcinoma patients undergoing extensive left-sided lymph node dissection: a retrospective observational study
- Shin Hwang, Dong-Hwan Jung, Eun-Kyoung Jwa, Yumi Kim
- J Yeungnam Med Sci. 2022;39(3):235-243. Published online December 14, 2021
- DOI: https://doi.org/10.12701/yujm.2021.01550
- 3,991 View
- 64 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Intrahepatic cholangiocarcinoma (ICC) of the left liver often shows left-sided lymph node (LN) metastasis. If gastric lesser curvature is extensively dissected, it can induce an iatrogenic injury to the extragastric vagus nerve branches that control motility of the pyloric sphincter and lead to gastric stasis. To cope with such LN dissection-associated gastric stasis, we performed pyloroplasty preemptively. The objective of this study was to analyze our 20-year experience of preemptive pyloroplasty performed in 10 patients.
Methods
We investigated clinical sequences of 10 patients with ICC who underwent preemptive pyloroplasty following left hepatectomy and extended left-sided LN dissection. Incidence of gastric stasis and oncological survival outcomes were analyzed.
Results
All 10 patients were classified as stage IIIB due to T1-3N1M0 stage according to the 8th edition of American Joint Committee on Cancer staging system. The overall patient survival rate was 51.9% at 1 year, 25.9% at 2 years, and 0% at 3 years. Seven patients showed uneventful postoperative recovery after surgery. Two patients suffered from gastric stasis, which was successfully managed with supportive care. One patient suffered from overt gastric paresis, which was successfully managed with azithromycin administration for 1 month.
Conclusion
We believe that preemptive pyloroplasty is an effective surgical option to prevent gastric stasis in patients undergoing extensive left-sided LN dissection. Azithromycin appears to be a potent prokinetic agent in gastroparesis. -
Citations
Citations to this article as recorded by- Clinical implications and optimal extent of lymphadenectomy for intrahepatic cholangiocarcinoma: A multicenter analysis of the therapeutic index
Yuzo Umeda, Kosei Takagi, Tatsuo Matsuda, Tomokazu Fuji, Toru Kojima, Daisuke Satoh, Masayoshi Hioki, Yoshikatsu Endo, Masaru Inagaki, Masahiro Oishi, Takahito Yagi, Toshiyoshi Fujiwara
Annals of Gastroenterological Surgery.2023; 7(3): 512. CrossRef
- Clinical implications and optimal extent of lymphadenectomy for intrahepatic cholangiocarcinoma: A multicenter analysis of the therapeutic index
- Effect of nonsurgical periodontal therapy and smoking status on hematological variables related to anemia of chronic disease in chronic periodontitis patient: a case-control study
- Sangita Show, Somen Bagchi, Arka Kanti Dey, Ramanarayana Boyapati, Pritish Chandra Pal, Kanikanti Siva Tejaswi
- J Yeungnam Med Sci. 2022;39(3):244-249. Published online May 16, 2022
- DOI: https://doi.org/10.12701/jyms.2022.00045

- 3,224 View
- 85 Download
- 1 Web of Science
-
 Abstract
Abstract
 PDF
PDF - Background
Chronic infectious, inflammatory, or neoplastic disorders are associated with anemia of chronic disease. Chronic inflammatory diseases such as periodontitis may contribute to masked anemia, especially in smokers. This study was aimed at verifying and comparing the efficacy of nonsurgical periodontal therapy (NSPT) for improving anemia among chronic periodontitis patients with and without the habit of smoking.
Methods
Thirty systemically healthy individuals with chronic periodontitis were divided into two groups of 15 each, smokers (group A) and nonsmokers (group B). The groups were compared based on hematological parameters such as serum erythropoietin (SE) and serum ferritin (SF) levels at baseline and 3 months after NSPT for anemia evaluation.
Results
The baseline SE levels in groups A and B were 11.84 and 15.19 mIU/mL (p=0.031), respectively; the corresponding levels at 3 months after NSPT were 13.00 and 17.74 mIU/mL (p=0.022). The baseline SF levels in groups A and B were 95.49 and 44.86 ng/mL (p=0.018), respectively; the corresponding levels at 3 months after NSPT were 77.06 and 39.05 ng/mL (p=0.009). Group B showed a significant increase and decrease in the SE and SF levels, respectively, at 3 months after NSPT (p=0.035 and p=0.039, respectively), whereas group A showed insignificant changes (p=0.253 and p=0.618, respectively).
Conclusion
NSPT led to an improvement in anemia among chronic periodontitis patients. However, the improvement is less in smokers compared to that in nonsmokers. Furthermore, SF and SE levels might serve as effective biomarkers for assessing anemia in smokers and nonsmokers with chronic periodontitis.
Case reports
- Pedunculated mucinous cystic neoplasm of the liver: a case report
- Sang-Woo Ha, Shin Hwang, Hyejin Han, Song Ie Han, Seung-Mo Hong
- J Yeungnam Med Sci. 2022;39(3):250-255. Published online August 3, 2021
- DOI: https://doi.org/10.12701/yujm.2021.01256

- 4,237 View
- 76 Download
-
 Abstract
Abstract
 PDF
PDF - In 2010, the World Health Organization classified mucin-producing bile duct tumors of the liver into two distinct entities; mucinous cystic neoplasm of the liver (MCN-L) and intraductal papillary mucinous neoplasm of the bile duct. We present the case of a patient with MCN-L having a uniquely pedunculated shape. A 32‐year‐old woman was referred to our institution with a diagnosis of biliary cystic neoplasm. She had undergone left salpingo-oophorectomy for ovarian cancer 15 years ago. Imaging studies showed an 8 cm-sized well defined, multiloculated cystic lesion suggesting a mucinous cystic neoplasm. The cystic mass was pedunculated at the liver capsule and pathologically diagnosed as MCN-L. The mass was resected with partial hepatectomy. The patient recovered uneventfully. She was discharged 7 days postoperatively. The patient has been doing well for 6 months after the operation. The patient will be followed up annually because of the favorable postresection prognosis of MCN-L.
- Primary hepatic sarcoidosis presenting with cholestatic liver disease and mimicking primary biliary cholangitis: a case report
- Young Joo Park, Hyun Young Woo, Moon Bum Kim, Jihyun Ahn, Jeong Heo
- J Yeungnam Med Sci. 2022;39(3):256-261. Published online August 10, 2021
- DOI: https://doi.org/10.12701/yujm.2021.01151

- 4,879 View
- 106 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Sarcoidosis often involves the liver. However, primary hepatic sarcoidosis confined to the liver without evidence of systemic involvement is rare. We report the case of a 37-year-old man with hepatic sarcoidosis who initially presented with elevated liver enzymes and suspicious cirrhotic nodules on computed tomography. The patient had cirrhosis but did not have portal hypertension. Based on the initial histopathologic finding of chronic granulomatous inflammation and the common clinical characteristics of sarcoidosis, he was initially diagnosed with primary biliary cholangitis, and his daily dosage of ursodeoxycholic acid was increased to 900 mg. After 14 months of treatment, his total serum bilirubin concentration was 10.9 mg/dL (upper normal limit, 1.2 mg/dL). Additionally, a transjugular liver biopsy revealed multiple noncaseating granulomas. He was diagnosed with primary hepatic sarcoidosis involving the lungs, heart, spleen, kidneys, and skin. Treatment with methylprednisolone was initiated. Two weeks later, he was started on azathioprine, and the dose of steroid was simultaneously reduced. These findings indicate the importance of including hepatic sarcoidosis as a possible diagnosis in patients with elevated liver enzymes or cryptogenic cirrhosis.
-
Citations
Citations to this article as recorded by- Liver biopsy as a useful diagnostic tool for hepatic sarcoidosis: A case report
Kenrei Uehara, Tatsuo Kanda, Shuhei Arima, Mai Totsuka, Masayuki Honda, Ryota Masuzaki, Reina Sasaki‑tanaka, Naoki Matsumoto, Masahiro Ogawa, Hirofumi Kogure
Medicine International.2024;[Epub] CrossRef - Navigating Challenges in a Case of Unusual Hepatic and Pulmonar Sarcoidosis: A Comprehensive Clinical Journey
André Gonçalves, Diogo Simas, Plácido Gomes, Carina Leal, Catarina Atalaia-Martins, Helena Vasconcelos
GE - Portuguese Journal of Gastroenterology.2024; : 1. CrossRef - The clinical management of hepatic sarcoidosis: A systematic review
Ram Prasad Sinnanaidu, Vikneshwaran Chandra Kumar, Ranita Hisham Shunmugam, Sanjiv Mahadeva
JGH Open.2024;[Epub] CrossRef
- Liver biopsy as a useful diagnostic tool for hepatic sarcoidosis: A case report
- Prolonged oral sildenafil use-induced Mondor disease: a case report
- Han Sol Chung, You Ho Mun
- J Yeungnam Med Sci. 2022;39(3):262-265. Published online May 24, 2022
- DOI: https://doi.org/10.12701/jyms.2022.00220

- 4,094 View
- 91 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Penile Mondor disease (MD) is a palpable, painful, subcutaneous induration caused by superficial dorsal penile vein thrombosis. We report a case of penile MD that was suspected to be related to prolonged oral sildenafil use. A 46-year-old man visited our emergency department with sustained penile pain and swelling that began 7 hours after sexual intercourse. He had used oral sildenafil intermittently for 11 years and engaged in sexual intercourse the previous night after taking sildenafil. Examination revealed no evidence of intercourse-related trauma to the genital area or an increase in penile skin temperature. However, penile swelling and tenderness over the protruding dorsal penile vein were noted. A color Doppler ultrasound examination was performed immediately, which showed hyperechoic thrombosis in the right superficial dorsal penile vein that was dilated, with soft tissue swelling and no detectable flow signal in the thrombotic lesion. The patient was diagnosed as having penile MD. The patient was treated conservatively. Some reports have indicated the involvement of sildenafil in thrombogenesis. Physicians should be aware that prolonged oral sildenafil use may be associated with penile MD.
-
Citations
Citations to this article as recorded by- A case with Penile Mondor’s disease
Hülya Cenk, Gülbahar Saraç, İrem Mantar Yanatma
TURKDERM.2023; : 151. CrossRef
- A case with Penile Mondor’s disease
Image vignette
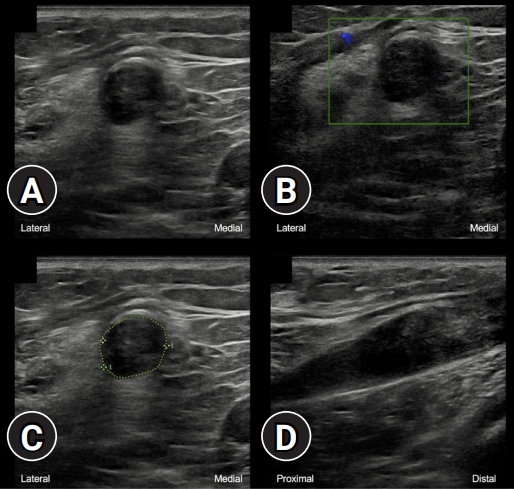
- Playing snakes and ladders with the common fibular nerve on ultrasound after knee dislocation
- Natan Bensoussan, Mathieu Boudier-Revéret, Johan Michaud
- J Yeungnam Med Sci. 2022;39(3):266-267. Published online September 15, 2021
- DOI: https://doi.org/10.12701/yujm.2021.01389
- 3,619 View
- 87 Download

 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine


 First
First Prev
Prev



