Abstract
-
Background
- Chromogranin A (CgA) levels have been reported to predict mortality in patients with heart failure. However, information on the prognostic value and clinical availability of CgA is limited. We compared the prognostic value of CgA to that of previously proven natriuretic peptide biomarkers in patients with acute heart failure.
-
Methods
- We retrospectively evaluated 272 patients (mean age, 68.5±15.6 years; 62.9% male) who underwent CgA test in the acute stage of heart failure hospitalization between June 2017 and June 2018. The median follow-up period was 348 days. Prognosis was assessed using the composite events of 1-year death and heart failure hospitalization.
-
Results
- In-hospital mortality rate during index admission was 7.0% (n=19). During the 1-year follow-up, a composite event rate was observed in 12.1% (n=33) of the patients. The areas under the receiver-operating characteristic curves for predicting 1-year adverse events were 0.737 and 0.697 for N-terminal pro-B-type natriuretic peptide (NT-proBNP) and CgA, respectively. During follow-up, patients with high CgA levels (>158 pmol/L) had worse outcomes than those with low CgA levels (≤158 pmol/L) (85.2% vs. 58.6%, p<0.001). When stratifying the patients into four subgroups based on CgA and NT-proBNP levels, patients with high NT-proBNP and high CgA had the worst outcome. CgA had an incremental prognostic value when added to the combination of NT-proBNP and clinically relevant risk factors.
-
Conclusion
- The prognostic power of CgA was comparable to that of NT-proBNP in patients with acute heart failure. The combination of CgA and NT-proBNP can improve prognosis prediction in these patients.
-
Keywords: Biomarkers; Chromogranin A; Heart failure; Prognosis
Introduction
- Heart failure (HF) is an increasing health problem worldwide [1-3]. Despite recent progress in pharmacologic and implantable cardiac device treatment, the mortality of patients with HF remains substantially high [2-6]. There is increasing interest in the use of many biological markers, including natriuretic peptides, to more accurately determine patient prognosis, such as mortality and HF hospitalization.
- Neurohormonal deterioration plays a key role in the development of HF. Numerous biomarkers and therapeutic approaches have been established to elucidate this pathophysiological mechanism. Natriuretic peptide has become a reliable biomarker for the diagnosis and estimation of prognosis in patients with HF. Additionally, the use of novel biomarkers may guarantee a more accurate estimation of the prognosis of HF and can be valuable for understanding the pathophysiology of HF. Chromogranin A (CgA) is a prohormone produced in many tissues, including neuroendocrine and myocardial tissues. The level of CgA is closely correlated with sympathetic activity in the adrenal gland and peripheral nervous system, suggesting that it might be a marker of sympathetic activity in humans [7]. In addition, it has been known as a biomarker for neuroendocrine tumors [8] and has recently been found to be associated with prognosis in patients with cardiovascular disease [9-12]. Recent studies have shown that CgA is an independent predictor of long-term mortality and HF hospitalization in patients with acute coronary syndromes [9]. In patients with HF, circulating CgA levels are associated with functional status, HF hospitalization, and mortality [10].
- The present study aimed to investigate (1) the prognostic value of CgA in patients with acute HF and (2) the additive prognostic impact of CgA when measured together with N-terminal pro-B-type natriuretic peptide (NT-proBNP) in patients with acute HF.
Materials and methods
- 1. Study population
- We retrospectively evaluated patients who underwent CgA testing during the acute stage of HF hospitalization between June 2017 and June 2018. A total of 272 patients were enrolled, and the median follow-up duration was 348 days.
- The diagnosis of HF was established based on current guidelines, taking into account symptoms, laboratory findings, and radiographic and echocardiographic findings.
- Data on demographic characteristics, medications, laboratory tests, and prognosis were collected from the patients’ medical charts. Initial transthoracic echocardiographic findings were collected from the images and reports from the database. NT-proBNP (The Dimension Vista PBNP Flex reagent cartridge; Erlangen, Germany) and CgA (Cisbio CgA ELISA kit; Codolet, France) were tested in venous blood and within 24 hours of hospital admission. Patients were followed up for 12 months after the index hospitalization. The primary endpoint was a composite event of 1-year death and hospitalization for HF. The death certificates and National Health Insurance data were reviewed to determine survival or death.
- 2. Statistics
- Data are presented as percentages for baseline characteristics and categorical variables, and comparisons between them were assessed using the chi-square test. The distribution of continuous variables is expressed as the mean±standard deviation or median (interquartile range), and the differences were compared using the independent t-test.
- A receiver-operating characteristic (ROC) curve was used to identify the optimal cutoff points for the CgA and NT-proBNP levels to determine the potential relationship between CgA and prognosis. Delong’s method was used to compare the area under the curves (AUCs) between CgA and NT-proBNP. All patients were classified into four groups according to the cutoff levels for NT-proBNP and CgA obtained from the ROC curve analysis. Kaplan-Meier survival analysis was performed based on these four groups. Bonferroni correction was used in the subgroup analysis that tested the prognostic value of CgA in patients with high and low NT-proBNP levels. All analyses were two-tailed, and p-values of <0.05 were considered statistically significant.
- The relationship between the two biomarkers and prognosis (composite outcome of 1-year death and hospitalization for HF) of the patients were investigated.
Results
- 1. Baseline characteristics
- Patients who underwent CgA and NT-proBNP testing between June 2017 and June 2018 in the acute stage of HF hospitalization were enrolled retrospectively. A total of 272 patients (mean age, 68.5±15.6 years; 62.9% male) were enrolled, and the median follow-up duration was 348 days. Nearly half of the patients had New York Heart Association (NYHA) class III–IV symptoms (45.2%). Of the total patients, 133 (48.9%) had hypertension, 86 (31.6%) had diabetes mellitus, 54 (19.9%) had atrial fibrillation, and 108 (39.7%) had ischemic heart disease. The mean left ventricular ejection fraction (LVEF) was 42.6%±16.1%, the mean NT-proBNP level was 10,650.1±26,302.4 pg/mL, and the mean CgA level was 279.8±392.6 pmol/L (Table 1). The CgA level increased with a decrease in LVEF and an increase in NYHA class (Supplementary Figs. 1, 2).
- Patients in both the high NT-proBNP and high CgA groups were more likely to be older and to be prescribed a loop diuretic in their discharge medications than those in the low NT-proBNP and low CgA groups. The high CgA group had higher NT-proBNP levels than the low CgA group. In addition, higher CgA levels were observed in the high NT-proBNP group than in the low NT-proBNP group. In the high CgA group, de novo HF was observed less frequently than in the low CgA group. Atrial fibrillation, ischemic heart disease, medication before admission, and estimated glomerular filtration rate were not different between the two groups regardless of NT-proBNP and CgA levels (Table 1, Supplementary Table 1).
- 2. Prognostic value of serum CgA and NT-proBNP
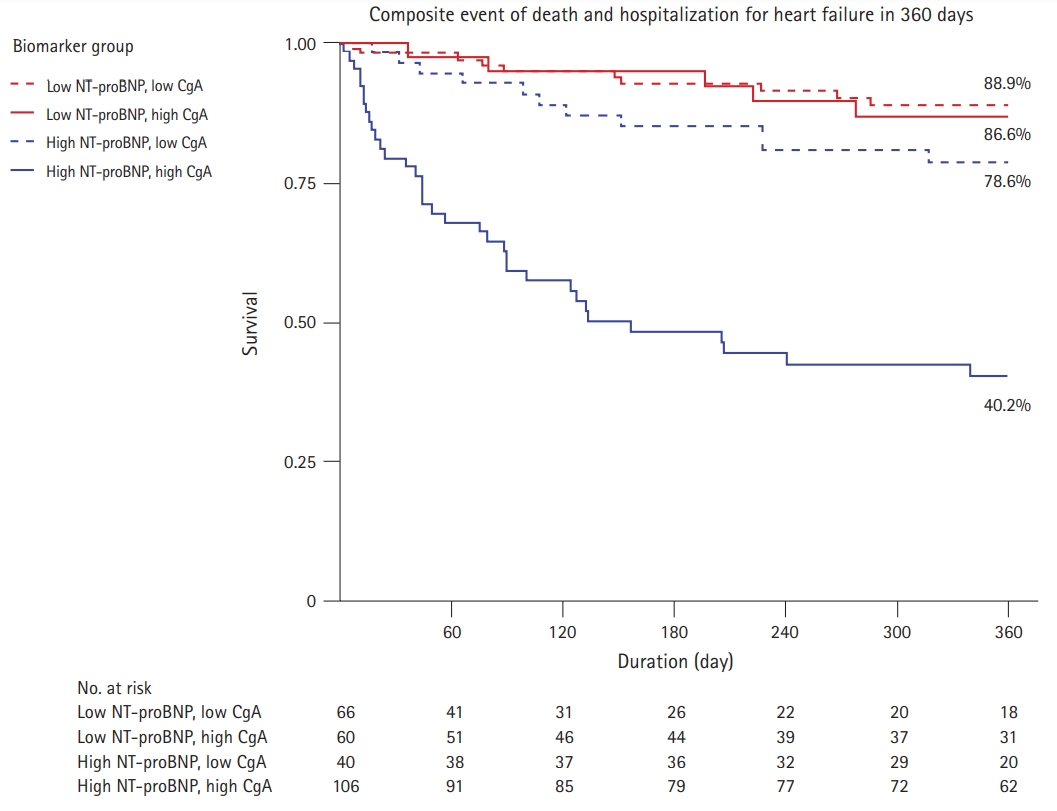
- In-hospital mortality rate of the study population was 7.0% (n=19). During the follow-up period, the composite event of 1-year death and hospitalization for HF was observed in 12.1% of patients (n=33). In the ROC analysis to predict the composite event of 1-year death and hospitalization, the AUCs were 0.737 and 0.697 for NT-proBNP and CgA, respectively. The cutoff values for predicting the prognosis for CgA and NT-proBNP were 158 pmol/L and 3,429 pg/mL, respectively (Fig. 1). During the follow-up, patients with high CgA (>158 pmol/L) were more likely to have worse outcomes (85.2% vs. 58.6%, p<0.001) in the Kaplan-Meier analysis. Age, NYHA class, atrial fibrillation, de novo HF, NT-proBNP level, and CgA level were significantly associated with prognosis in the univariate analysis. In the multivariable analysis model, CgA was an independent factor associated with 1-year death and hospitalization for HF (hazard ratio [HR], 1.059/100 pmol/L; 95% confidence interval [CI], 1.007–1.115, p=0.027), as was age, NYHA class, and de novo HF (Table 2).
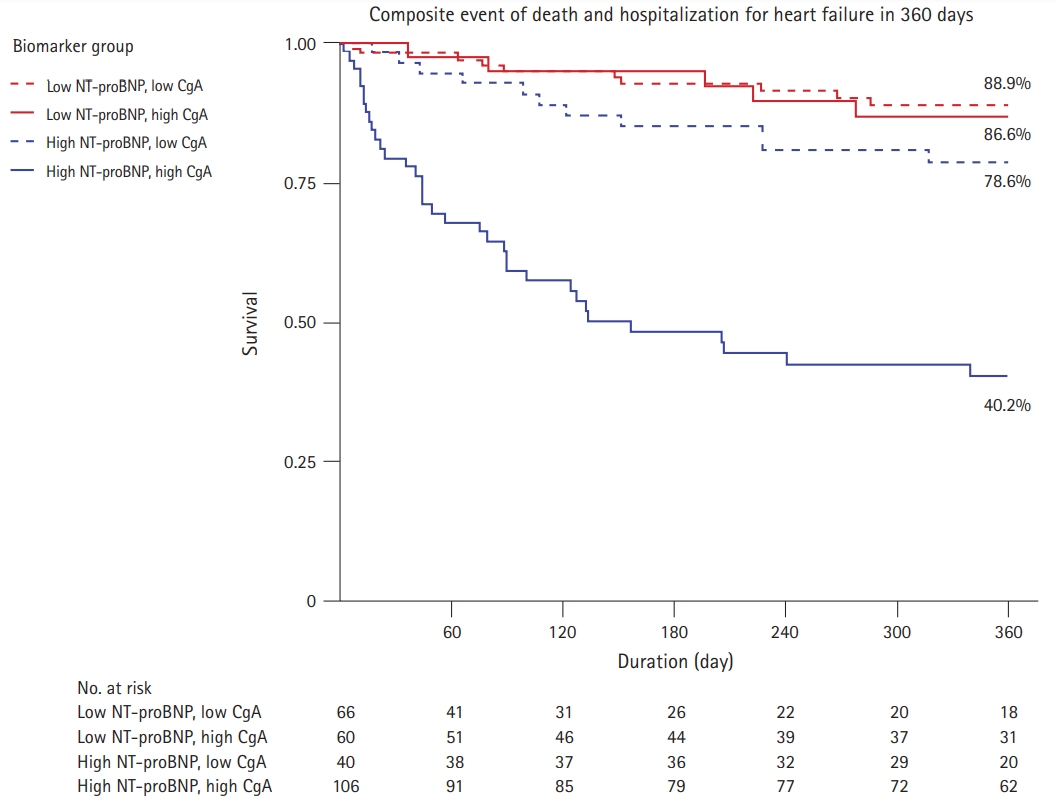
- Based on the cutoff values for CgA (158 pmol/L) and NT-proBNP (3,429 pg/mL), the study cohort was divided into four groups: low NT-proBNP and low CgA (n=106), low NT-proBNP and high CgA (n=40), high NT-proBNP and low CgA (n=60), and high NT-proBNP and high CgA (n=66). The Kaplan-Meier survival analysis showed that the group with low levels of both NT-proBNP and CgA had the best 1-year survival rate (88.9%), followed by the group with low NT-proBNP and high CgA levels (86.6%), the group with high NT-proBNP and low CgA levels (78.6%), and the group with both high NT-proBNP and CgA levels (40.2%, p<0.001) (Fig. 2). In the subgroup of patients with high NT-proBNP levels, low CgA levels were associated with patient prognosis (40.2% vs. 78.6%, p<0.001), whereas there was no significant prognostic value in the subgroup of patients with low NT-proBNP levels (86.6% vs. 88.9%, p>0.999).
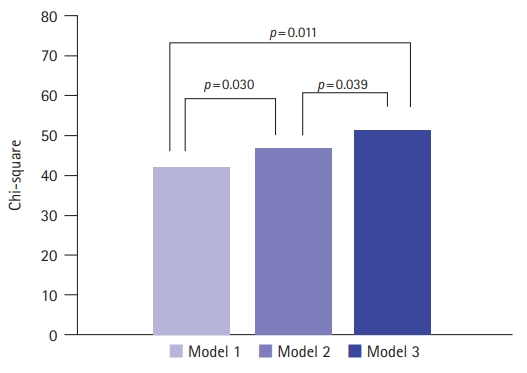
- To investigate the predictive value of CgA, we created three models: (1) the baseline model including the risk factors of age, sex, NYHA class, atrial fibrillation, and de novo HF; (2) baseline model+NT-proBNP; and (3) baseline model+NT-proBNP+CgA. The addition of serum NT-proBNP and CgA to the established risk factors increased the provided incremental information for predicting the prognosis (global chi-square 42.4 to 47.2, p=0.030). Adding CgA to the second model, which comprised both the established risk factors and NT-proBNP, resulted in additional improvement of the prognostic power for 1-year adverse events (global chi-square from 47.2 to 51.4, p=0.039) (Fig. 3).
Discussion
- In the present study, blood CgA levels in patients with acute HF were found to be an independent factor associated with 1-year death and hospitalization for HF. We divided the study cohort into four groups based on NT-proBNP and CgA blood concentrations. Those with low NT-proBNP and low CgA levels showed the lowest rates of 1-year death and hospitalization for HF. High NT-proBNP and high CgA levels were associated with the worst outcomes. Our findings demonstrate the advantage of adding CgA levels to a well-established biomarker, NT-proBNP, for better risk stratification. Simultaneous measurement of NT-proBNP and CgA can help predict death in patients with acute HF more accurately than the estimation of NT-proBNP alone. In particular, CgA has a low significance as a prognostic predictor of 1-year death and HF hospitalization in patients with low NT-proBNP levels and may be more helpful as a prognostic predictor in patients with high NT-proBNP levels. In our study, the high NT-proBNP group was older and consisted of a greater proportion of individuals with NYHA class III–IV, suggesting that CgA may be more helpful in predicting the prognosis of high-risk groups of patients with acute HF.
- Ceconi et al. [10] suggested that CgA levels were increased in patients with chronic HF and were a predictor of mortality. Røsjø et al. [13] investigated the prognostic value of CgA in patients with stabilized HF from the GISSI-Heart Failure trial. In the univariable analysis, increased CgA plasma concentrations were associated with all-cause mortality, with hazard ratios between 1.58 (95% CI, 1.17–2.11) and 2.35 (95% CI, 1.78–3.10). However, after adjustment for clinically relevant risk factors, the association was not significant.
- A recent study investigated the underlying mechanism of CgA increase in patients with acute HF, suggesting a role for CgA in patients with acute HF [11]. CgA is a member of the granin protein family, which plays a role in the endocrine and paracrine system and seems to play a role in cardiovascular disease. One of the mechanisms of increased CgA in patients with HF is thought to be the impaired processing of CgA to CgA fragment catestatin [11]. Ottesen et al. [11] revealed that the fragment catestatin may directly dysregulate cardiomyocyte Ca2+ handling, indicating that elevated CgA can be related to patient prognosis in the acute stage of HF.
- NT-proBNP is a well-established biomarker in a variety of heart diseases, including HF, because of its correlation with clinical status, echocardiographic parameters, laboratory findings, and short-term and long-term prognosis [14-16]. NT-proBNP is a neurohormone released by the ventricles of the heart as a result of volume or pressure overload and has a different mechanism than CgA secretion. Our study indicates that when biomarkers from two different mechanisms are combined, they are synergistic in predicting the long-term prognosis of patients with acute HF. The simultaneous application of CgA and NT-proBNP allows a more accurate estimate of the prognosis of patients with acute HF in clinical practice.
- Our study had some limitations to consider. First, this was a relatively small retrospective study conducted in a single center. Thus, the results of the present study need to be validated in larger trials. Second, although we included all patients available during the index period, there may have been some selection bias in [2,17] the study population.
- CgA presented prognostic power comparable to that of the proven biomarker NT-proBNP in patients with acute HF. CgA combined with NT-proBNP levels demonstrated an additive prognostic value in these patients.
Supplementary materials
Supplementary materials can be found via https://doi.org/10.12701/yujm.2020.00843
Supplementary Fig. 1.
Chromogranin A (CgA) levels according to the left ventricular ejection fraction (LVEF) group. CgA levels were the highest in the LVEF <40% group.
yujm-2020-00843-suppl2.pdf
Supplementary Fig. 2.
The levels of chromogranin A (CgA) according to the New York Heart Association (NYHA) functional class. As NYHA functional class worsens, a positive correlation with CgA levels is observed.
yujm-2020-00843-suppl3.pdf
Notes
-
Ethical statements
The Institutional Review Board (IRB) of Kyungpook National University Hospital approved this study and permitted the review and publication of patient records (IRB No: 2019-12-017-001). All data were anonymized before analysis, and the need for written informed consent was waived by the IRB due to the retrospective nature of this study.
-
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
-
Funding
This research was supported by the Kyungpook National University Research Fund (2020).
-
Author contributions
Conceptualization: DHY, BEP, YJP, HJK, SYJ, MHB, JHL, HSP, YC, SCC; Investigation: BEP, YJP, HJK; Data curation: HNK, DHY, BEP, YJP, HJK; Formal analysis: HNK, DHY, SYJ, MHB, HSP, YC, SCC; Funding acquisition, Validation: DHY, SYJ, JHL, HSP, YC, SCC; Methodology: DHY, SYJ, MHB, JHL, YC; Project administration: DHY; Supervision: DHY, SYJ, MHB, HSP, YC, SCC; Writing-original draft: HNK, YJP; Writing-review & editing: HNK, DHY, BEP, SYJ, MHB, JHL, HSP.
Fig. 1.Receiver-operating characteristic curve analysis of N-terminal pro-B-type natriuretic peptide (NT-proBNP) and chromogranin A (CgA) in predicting the composite outcome of 1-year death and hospitalization for heart failure. The cutoff values for CgA and NT-proBNP were 158 pmol/L and 3,429 pg/mL, respectively. Areas under the curves for CgA and NT-proBNP levels in predicting 1-year death and hospitalization were 0.697 and 0.737, respectively.
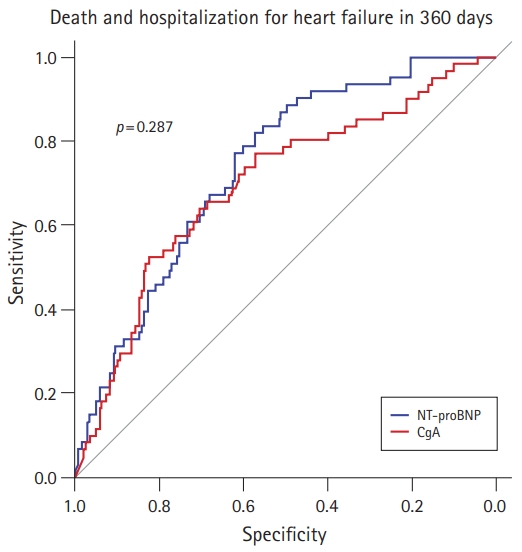
Fig. 2.Kaplan-Meier survival analysis of the groups according to the levels of chromogranin A (CgA; cutoff value=158 pmol/L) and N-terminal pro-B-type natriuretic peptide (NT-proBNP; cutoff value=3,429 pg/mL).
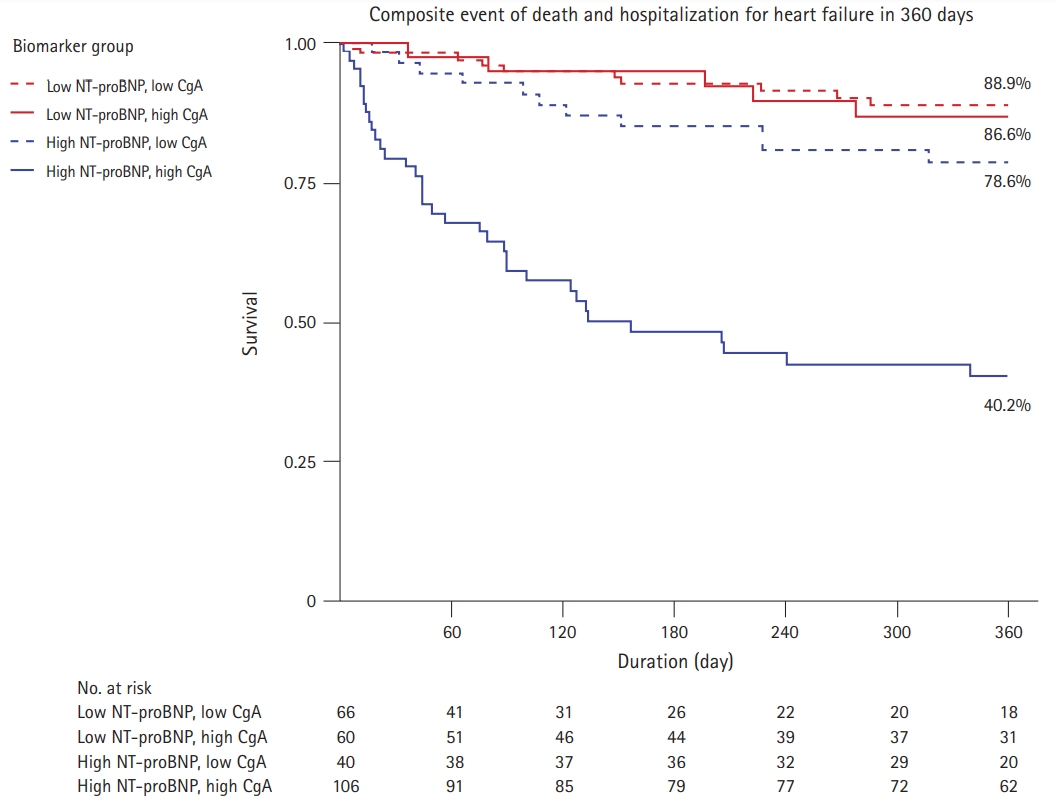
Fig. 3.Comparison among the models including the established risk factors, N-terminal pro-B-type natriuretic peptide (NT-proBNP), and chromogranin A (CgA) in predicting 1-year mortality. Model 1 includes age, sex, New York Heart Association (NYHA) class, atrial fibrillation, and de novo heart failure. Model 2: model 1+NT-proBNP. Model 3: model 2+CgA.
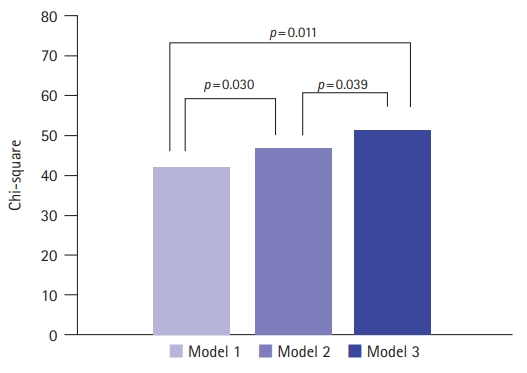
Table 1.Baseline characteristics of the patients according to level of serum NT-proBNP and CgA
|
Variable |
|
NT-proBNP
|
CgA
|
|
All (n=272) |
Low (n=146) |
High (n=126) |
p-value |
Low (n=166) |
High (n=106) |
p-value |
|
Demographics |
|
|
|
|
|
|
|
|
Age (yr) |
68.5±15.6 |
66.7±15.5 |
70.5±15.5 |
0.040 |
65.7±16.6 |
72.8±12.9 |
<0.001 |
|
Male sex |
171 (62.9) |
92 (63.0) |
79 (62.7) |
>0.999 |
110 (66.3) |
61 (57.5) |
0.186 |
|
Hypertension |
133 (48.9) |
64 (43.8) |
69 (54.8) |
0.094 |
61 (36.7) |
72 (67.9) |
<0.001 |
|
Diabetes mellitus |
86 (31.6) |
39 (26.7) |
47 (37.3) |
0.081 |
37 (22.3) |
49 (46.2) |
<0.001 |
|
Atrial fibrillation |
54 (19.9) |
27 (18.5) |
27 (21.4) |
0.651 |
32 (19.3) |
22 (20.8) |
0.887 |
|
De novo heart failure |
204 (75.0) |
119 (81.5) |
85 (67.5) |
0.011 |
132 (79.5) |
72 (67.9) |
0.044 |
|
NYHA class |
|
|
|
<0.001 |
|
|
0.256 |
|
II |
149 (54.8) |
106 (72.6) |
43 (34.1) |
|
94 (56.6) |
55 (51.9) |
|
|
III |
65 (23.9) |
23 (15.8) |
42 (33.3) |
|
42 (25.3) |
23 (21.7) |
|
|
IV |
58 (21.3) |
17 (11.6) |
41 (32.5) |
|
30 (18.1) |
28 (26.4) |
|
|
Ischemic etiology |
108 (39.7) |
59 (40.4) |
49 (38.9) |
0.859 |
64 (38.6) |
44 (41.9) |
0.673 |
|
SBP (mmHg) |
135.5±30.2 |
133.1±28.3 |
138.3±32.2 |
0.155 |
132.2±28.1 |
140.6±32.8 |
0.024 |
|
Heart rate (beat/min) |
88.6±22.5 |
84.0±20.4 |
94.0±23.7 |
<0.001 |
86.8±21.0 |
91.4±24.5 |
0.101 |
|
Laboratory findings |
|
|
|
|
|
|
|
|
Hemoglobin (g/dL) |
12.6±2.1 |
12.4±2.3 |
12.8±2.0 |
0.126 |
12.5±2.2 |
12.8±2.0 |
0.404 |
|
Serum creatinine (mg/dL) |
2.0±9.4 |
2.5±12.8 |
1.3±1.0 |
0.244 |
2.3±11.9 |
1.4±2.1 |
0.337 |
|
eGFR (mL/min/1.73 m2) |
78.0±191.9 |
87.5±260.7 |
67.0±31.6 |
0.351 |
64.5±30.3 |
99.1±304.5 |
0.248 |
|
Sodium (mEq/L) |
137.3±6.0 |
137.3±6.0 |
137.4±6.0 |
0.913 |
137.6 ±6.2 |
137.0±5.7 |
0.405 |
|
Potassium (mEq/L) |
4.3±0.6 |
4.2±0.6 |
4.3±0.6 |
0.459 |
4.3±0.6 |
4.2±0.6 |
0.354 |
|
CgA (pmol/L) |
279.8±392.6 |
160.1±222.2 |
418.5±490.8 |
<0.001 |
81.2±38.7 |
590.9±485.2 |
<0.001 |
|
NT-proBNP (pg/mL) |
10,650.1±26,302.4 |
1,204.1±1,024.7 |
21,595.4±35,688.4 |
<0.001 |
4,336.4±6,456.9 |
20,537.6±39,475.4 |
<0.001 |
|
LVEF group (%) |
|
|
|
<0.001 |
|
|
0.058 |
|
≥50 |
114 (41.9) |
86 (58.9) |
28 (22.2) |
|
79 (47.6) |
35 (33.0) |
|
|
40–49 |
43 (15.8) |
27 (18.5) |
16 (12.7) |
|
23 (13.9) |
20 (18.9) |
|
|
<40 |
115 (42.3) |
33 (22.6) |
82 (65.1) |
|
64 (38.6) |
51 (48.1) |
|
|
LVEF (%) |
42.6±16.1 |
48.9±14.0 |
35.4±15.5 |
<0.001 |
43.7±16.7 |
41.0±15.1 |
0.178 |
|
Renal replacement therapy |
7 (2.6) |
0 (0) |
7 (5.6) |
0.012 |
1 (0.6) |
6 (5.7) |
0.030 |
Table 2.Univariable and multivariable analysis for prediction of composite event of 1-year death and hospitalization for heart failure
|
Variable |
Univariate model
|
Multivariate model
|
|
HR (95% CI) |
p-value |
HR (95% CI) |
p-value |
|
Age |
1.038 (1.016–1.059) |
<0.001 |
1.033 (1.010–1.056) |
0.005 |
|
Male sex |
0.962 (0.570–1.622) |
0.909 |
1.343 (0.771–2.340) |
0.298 |
|
Hypertension |
1.194 (0.723–1.974) |
0.488 |
|
|
|
Diabetes mellitus |
1.267 (0.751–2.137) |
0.375 |
|
|
|
Atrial fibrillation |
2.271 (1.330–3.877) |
0.003 |
1.784 (1.029–3.093) |
0.394 |
|
De novo onset |
0.329 (0.199–0.544) |
<0.001 |
0.439 (0.259–0.744) |
0.002 |
|
NYHA class III (reference, NYHA class II) |
1.735 (0.932–3.230) |
0.082 |
1.225 (0.636–2.362) |
0.543 |
|
NYHA class IV (reference, NYHA class II) |
2.861 (1.578–5.187) |
0.001 |
1.980 (1.051–3.729) |
0.035 |
|
Ischemic etiology |
0.989 (0.608–1.680) |
0.966 |
|
|
|
SBP (/10 mmHg) |
1.010 (0.932–1.095) |
0.804 |
|
|
|
Heart rate (/10 beats/minute) |
1.111 (0.993–1.244) |
0.066 |
|
|
|
Hemoglobin (g/dL) |
1.000 (0.882–1.131) |
0.984 |
|
|
|
eGFR (/10 mL/min/1.73 m2) |
1.012 (0.930–1.050) |
0.696 |
|
|
|
Renal replacement therapy |
2.573 (0.933–7.10) |
0.068 |
|
|
|
Sodium (/10 mEq/L) |
1.035 (0.693–1.544) |
0.868 |
|
|
|
Potassium (/10 mEq/L) |
0.660 (0.011–40.850) |
0.844 |
|
|
|
LVEF (%) |
0.996 (0.980–1.012) |
0.590 |
|
|
|
NT-proBNP (/10,000 pg/mL) |
1.096 (1.047–1.147) |
<0.001 |
1.051 (0.994–1.111) |
0.081 |
|
CgA (/100 pmol/L) |
1.096 (1.050–1.145) |
<0.001 |
1.059 (1.007–1.115) |
0.027 |
References
- 1. Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation 2019;139:e56–528.PubMed
- 2. Lee SE, Lee HY, Cho HJ, Choe WS, Kim H, Choi JO, et al. Clinical characteristics and outcome of acute heart failure in Korea: results from the Korean Acute Heart Failure Registry (KorAHF). Korean Circ J 2017;47:341–53.ArticlePubMedPMC
- 3. Ahn MS, Yoo BS, Yoon J, Lee SH, Kim JY, Ahn SG, et al. Prognostic effect of guideline-directed therapy is more noticeable early in the course of heart failure. J Korean Med Sci 2019;34:e133.ArticlePubMedPMC
- 4. Kim MS, Lee JH, Kim EJ, Park DG, Park SJ, Park JJ, et al. Korean Guidelines for Diagnosis and Management of Chronic Heart Failure. Korean Circ J 2017;47:555–643.ArticlePubMedPMC
- 5. Lee JH, Kim MS, Yoo BS, Park SJ, Park JJ, Shin MS, et al. KSHF Guidelines for the Management of Acute Heart Failure: Part II. Treatment of acute heart failure. Korean Circ J 2019;49:22–45.ArticlePubMed
- 6. Lee JH, Kim MS, Kim EJ, Park DG, Cho HJ, Yoo BS, et al. KSHF Guidelines for the Management of Acute Heart Failure: Part I. Definition, epidemiology and diagnosis of acute heart failure. Korean Circ J 2019;49:1–21.ArticlePubMed
- 7. Cryer PE, Wortsman J, Shah SD, Nowak RM, Deftos LJ. Plasma chromogranin A as a marker of sympathochromaffin activity in humans. Am J Physiol 1991;260(2 Pt 1):E243–6.ArticlePubMed
- 8. Eriksson B, Arnberg H, Oberg K, Hellman U, Lundqvist G, Wernstedt C, et al. Chromogranins: new sensitive markers for neuroendocrine tumors. Acta Oncol 1989;28:325–9.ArticlePubMed
- 9. Jansson AM, Røsjø H, Omland T, Karlsson T, Hartford M, Flyvbjerg A, et al. Prognostic value of circulating chromogranin A levels in acute coronary syndromes. Eur Heart J 2009;30:25–32.ArticlePubMed
- 10. Ceconi C, Ferrari R, Bachetti T, Opasich C, Volterrani M, Colombo B, et al. Chromogranin A in heart failure; a novel neurohumoral factor and a predictor for mortality. Eur Heart J 2002;23:967–74.ArticlePubMed
- 11. Ottesen AH, Carlson CR, Louch WE, Dahl MB, Sandbu RA, Johansen RF, et al. Glycosylated chromogranin A in heart failure: implications for processing and cardiomyocyte calcium homeostasis. Circ Heart Fail 2017;10:e003675.PubMed
- 12. Estensen ME, Hognestad A, Syversen U, Squire I, Ng L, Kjekshus J, et al. Prognostic value of plasma chromogranin A levels in patients with complicated myocardial infarction. Am Heart J 2006;152:927.Article
- 13. Røsjø H, Masson S, Latini R, Flyvbjerg A, Milani V, La Rovere MT, et al. Prognostic value of chromogranin A in chronic heart failure: data from the GISSI-Heart Failure trial. Eur J Heart Fail 2010;12:549–56.ArticlePubMed
- 14. Kantar M, Levent E, Cetingul N, Ulger Z, Ozyurek R, Aksoylar S, et al. Plasma natriuretic peptides levels and echocardiographic findings in late subclinical anthracycline toxicity. Pediatr Hematol Oncol 2008;25:723–33.ArticlePubMed
- 15. Bhalla V, Willis S, Maisel AS. B-type natriuretic peptide: the level and the drug: partners in the diagnosis of congestive heart failure. Congest Heart Fail 2004;10(1 Suppl 1):3–27.ArticlePubMed
- 16. Huang B, Shen J, Li L, Huang Y, Luo S. Effect of B-type natriuretic peptide level on long-term outcome in patients with end-stage heart failure. Am J Cardiol 2016;118:383–8.ArticlePubMed
- 17. Kim MS, Lee JH, Cho HJ, Cho JY, Choi JO, Hwang KK, et al. KSHF Guidelines for the Management of Acute Heart Failure: Part III. Specific management of acute heart failure according to the etiology and co-morbidity. Korean Circ J 2019;49:46–68.ArticlePubMed
Citations
Citations to this article as recorded by

- The Role of Congestion Biomarkers in Heart Failure with Reduced Ejection Fraction
Michele Correale, Francesco Fioretti, Lucia Tricarico, Francesca Croella, Natale Daniele Brunetti, Riccardo M. Inciardi, Anna Vittoria Mattioli, Savina Nodari
Journal of Clinical Medicine.2023; 12(11): 3834. CrossRef - Novel Biomarkers of Renal Dysfunction and Congestion in Heart Failure
Agata Zdanowicz, Szymon Urban, Barbara Ponikowska, Gracjan Iwanek, Robert Zymliński, Piotr Ponikowski, Jan Biegus
Journal of Personalized Medicine.2022; 12(6): 898. CrossRef

 , Dong Heon Yang1,2,3
, Dong Heon Yang1,2,3 , Bo Eun Park1
, Bo Eun Park1 , Yoon Jung Park1
, Yoon Jung Park1 , Hyeon Jeong Kim1
, Hyeon Jeong Kim1 , Se Yong Jang1,2,3
, Se Yong Jang1,2,3 , Myung Hwan Bae1,3
, Myung Hwan Bae1,3 , Jang Hoon Lee1,3
, Jang Hoon Lee1,3 , Hun Sik Park1,3
, Hun Sik Park1,3 , Yongkeun Cho1,3
, Yongkeun Cho1,3 , Shung Chull Chae1,3
, Shung Chull Chae1,3



 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine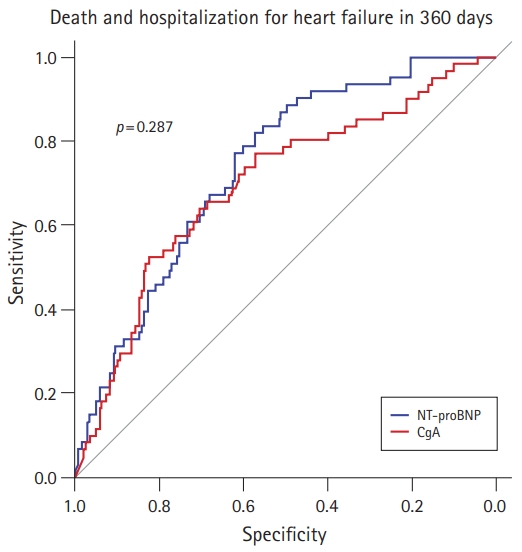
 PubReader
PubReader ePub Link
ePub Link Cite
Cite