Abstract
-
Background
- To date, there have been no studies on the normal anatomic values of the anal sphincter in healthy Koreans. Therefore, this study aimed to determine the normal anatomic values of transanal ultrasonography (TAUS).
-
Methods
- The thickness of the external anal sphincter (EAS) and internal anal sphincter (IAS) was measured by TAUS from healthy Korean volunteers between September 2019 and August 2021.
-
Results
- Thirty-six volunteers with a median age of 37 years (range, 20–77 years) and a median body mass index (BMI) of 23.5 kg/m2 (range, 17.2–31.2 kg/m2) were examined. The median thickness of the EAS at 4 cm and 2 cm from the anal verge was 7.4 mm (range, 5.8–8.8 mm) and 6.5 mm (range, 5.6–8.0 mm), respectively. The median thickness of the IAS at 2 cm from the anal verge was 1.8 mm (range, 0.8-4.3 mm). There were no differences in sphincter muscle thickness between the sexes. However, the EAS tended to thicken as the BMI increased (EAS at 2 cm and 4 cm from the anal verge, Spearman rho=0.433, 0.363; p=0.008 and p=0.029, respectively).
-
Conclusion
- In healthy Korean, the median thickness of the IAS at 2 cm from the anal verge was 1.8 mm and the median thickness of the EAS at 2 cm and 4 cm from the anal verge was 6.5 mm and 7.4 mm respectively. There were no differences in anal sphincter thickness between sexes, but BMI was related to EAS thickness.
-
Keywords: Anal canal; Anal sphincter; Anus; Ultrasonography
Introduction
- According to data from the Korean Statistical Information Service, 183,908 patients underwent hemorrhoidectomy in Korea in 2019, ranking it the third most frequent surgery [1]. As such, a representative and essential test for diagnosing anal disease, which is one of the most frequent diseases, is transanal ultrasonography (TAUS). TAUS is a useful test for examining the anatomical structure of the anus [2,3]. The advantage of TAUS is that it has no risk of radiation exposure and is less expensive than magnetic resonance imaging (MRI). In addition, TAUS can be easily performed in outpatient clinics.
- Anatomical deterioration, such as anal fistulas, abscesses, and sphincter defects, can be easily detected on TAUS by ultrasound-skilled clinicians [4]. In contrast, most diseases, such as fecal incontinence, constipation, or simple hemorrhoids, show no anatomical deterioration on TAUS. However, the absence of anatomical deterioration on TAUS does not indicate a normal finding. This is because the thickness of the sphincter and the degree of ultrasound shadowing may appear differently depending on the patient’s age, sex, past history, or degree of symptoms.
- Indeed, according to previous studies conducted in Western countries, the thickness of the internal sphincter is measured differently according to age, and there is a difference in the length of the anal canal and thickness of the external sphincter according to sex [4-6]. In addition, the results may vary depending on the observer [5-7].
- However, until now, there have been no studies on the normal anatomic value of the anal sphincter on TAUS in Koreans with no anal disease or symptoms. Therefore, research is needed to establish normal anatomic values for TAUS in healthy Koreans. The purpose of this study was to determine those normal values.
Materials and methods
-
Ethical statements: This study was approved by the Institutional Review Board (IRB) of Yeungnam University Hospital (IRB No: 2019-09-062-008) and all the subjects included in this study provided written informed consent.
- This prospective study was conducted in a tertiary medical center and local colorectal clinic in Daegu, Korea between September 2019 and August 2021.
- Healthy Korean adult volunteers who had no anal disease and symptoms were recruited through research subject recruitment notices on bulletin boards in hospitals, subways, and buses. The inclusion criteria were as follows: (1) age of ≥20 years, (2) no anorectal symptoms, (3) Wexner score of ≤2, and (4) no anorectal surgical history. The applicant’s participation in the study was finally decided through an interview and physical examination with the researcher. If asymptomatic anatomical deterioration was found during TAUS, the subject was excluded from the study.
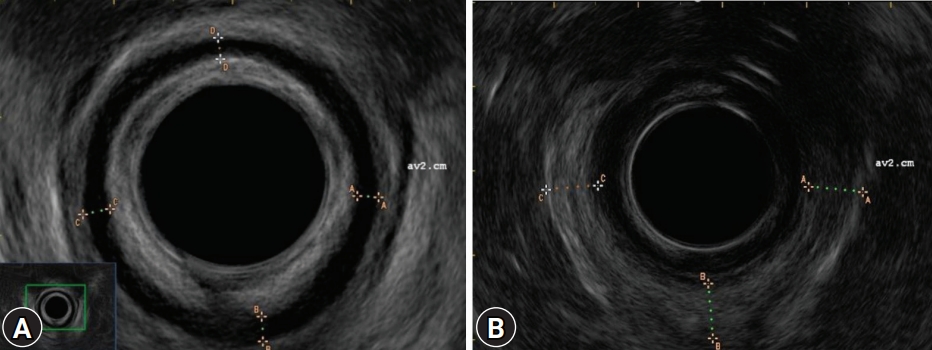
- TAUS was performed using an endorectal probe (ALBIT ultrasound scanner, anorectal rotating 360, R510; ECHO-SON, Ltd., Puławy, Poland) at a frequency of 7.5 and 12 MHz by an experienced colorectal surgeon (DS) (Fig. 1). An enema or bowel preparation drug was not administered prior to TAUS. The subject lay in the left lateral position, and serial radial images were acquired throughout the anal canal. The thickness of the internal anal sphincter (IAS) was measured in the direction of 12 o’clock (anterior), 3 o’clock (left lateral), 6 o’clock (posterior), and 9 o’clock (right lateral) at 2 cm from the anal verge (Fig. 2A). The thickness of the external anal sphincter (EAS) was measured in the direction of 3 o’clock (left lateral), 6 o’clock (posterior), and 9 o’clock (right lateral) at 2 cm and 4 cm from the anal verge (Fig. 2B).
- Non-normally distributed data, presented as median (range), were analyzed using the Mann-Whitney U-test. Correlations between variables were analyzed using Spearman rank correlation test. Statistical significance was set at p-value of <0.05. Statistical analyses were performed using IBM SPSS ver. 22.0 (IBM Corp., Armonk, NY, USA).
Results
- Thirty-six volunteers were examined for anal anatomy using TAUS. The median age of the subjects was 37 years (range, 20-77 years) and the median body mass index (BMI) was 23.5 kg/m2 (range, 17.2–31.2 kg/m2). Nineteen patients (52.8%) were male. The age distribution was 21 to 30 years (7 individuals, 19.4%), 31 to 40 years (14 individuals, 38.9%), 41 to 50 years (5 individuals, 13.9%), 51 to 60 years (5 individuals, 13.9%), 61 to 70 years (4 individuals, 11.1%), and 71 to 80 years (1 individual, 2.8%). The demographic characteristics of the study participants are presented in Table 1.
- The median thickness of the EAS at 4 cm and 2 cm from the anal verge was 7.4 mm (range, 5.8–8.8 mm) and 6.5 mm (range, 5.6–8.0 mm), respectively. The median thickness of the IAS at 2 cm from the anal verge was 1.8 mm (range, 0.8–4.3 mm).
- There were no differences in sphincter muscle thicknesses between male and female patients (Table 2, Fig. 3). However, the EAS tended to thicken as the BMI increased (EAS at 2 cm and 4 cm from the anal verge, Spearman rho=0.433 and 0.363; p=0.008 and 0.029, respectively) (Fig. 4).
Discussion
- In this study, we report a normal value of anal sphincter thickness in healthy Koreans as measured by TAUS. TAUS is the most frequently used examination for detecting anorectal anatomical variants because it can easily be performed in outpatient clinics without radiation exposure. Only a few studies have described the normal value of anal sphincter thickness in healthy adults [5,6,8,9]. However, all these studies were conducted in Western countries, and there have been no studies on healthy Asian or Korean volunteers.
- In our study, the median IAS thickness at 2 cm from the anal verge was 1.8 mm. This is consistent with the results of previous studies conducted in Western countries (2 mm; range, 1–3 mm) [9]. Although the median value in our study was thinner than that in the cited study, this difference was not considered meaningful because of the measurement error and range.
- The median EAS thickness in our study was 6.5 mm (range, 5.9–8.0 mm) at 2 cm from the anal verge. This is also consistent with the results of a previous study (6 mm; range, 5–8 mm) [9]. Unlike in the cited study, we also described the thickness of the EAS at the upper part of the anal canal (4 cm from the anal verge). The median EAS thickness of the upper anal canal was greater than that of the mid-anal cannula, although the difference was not statistically significant.
- In the present study, no relationship was found between sex and sphincter thickness. This result is also consistent with that of a previous study [5]. However, interestingly, BMI correlated with EAS thickness in our study. The higher the BMI, the thicker the EAS was; however, IAS thickness was not correlated with BMI. A previous report revealed that BMI was not correlated with IAS thickness on MRI [10]. However, the investigators did not examine EAS thickness in that study. Another study revealed that BMI was correlated with IAS and EAS thickness [11]. However, the BMI correlation differed according to the measuring level of the anal canal. Interestingly, the investigators revealed that BMI was negatively correlated with EAS thickness, which was the opposite of our result. However, as the previous study was conducted with only females and our study was conducted with a small sample size, further studies are needed to clarify the correlation between BMI and anal sphincter thickness.
- Our study has some limitations. First, the sample size was small. More than 80 participants were recruited at the beginning of the study. However, it was challenging to recruit healthy volunteers due to the outbreak of coronavirus disease 2019 at the beginning of the study. Therefore, the final sample size for this study was smaller than originally intended. Second, due to the small number of samples, we could not investigate the relationship between age and sphincter thickness. Third, we did not describe sphincter tone, which is possibly related to the thickness of the anal sphincter muscle. However, previous studies have reported no correlation between sphincter thickness and anal canal pressure [7]. Fourth, we could not measure the length of the anal sphincter muscle because of the limitations of the two-dimensional scope. Nevertheless, we believe that this study is meaningful as the first study to elucidate normal TAUS values in healthy Koreans.
- In this study, in healthy Korean volunteers, the median thickness of the IAS 2 cm from the anal verge was 1.8 mm, and the median thickness of the EAS at 2 cm and 4 cm from the anal verge was 6.5 mm and 7.4 mm, respectively, as measured by TAUS. There were no differences in anal sphincter thickness between sexes, but BMI was related to anal sphincter thickness. Further large-scale studies are required to confirm the results.
Notes
-
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
-
Funding
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (No. 2019R1G1A1097554).
-
Author contributions
Conceptualization, Investigation, Data curation, Formal analysis, Funding acquisition, Methodology, Visualization, Supervision: all authors; Project administration, Resources, Software: SIK; Writing-original draft: DS, SIK; Writing-review & editing: all authors.
Fig. 1.Endorectal probe (ALBIT ultrasound scanner, anorectal rotating 360, R510; ECHO-SON, Ltd., Puławy, Poland).

Fig. 2.(A) Internal anal sphincter and (B) external anal sphincter on transanal ultrasonography imaging.
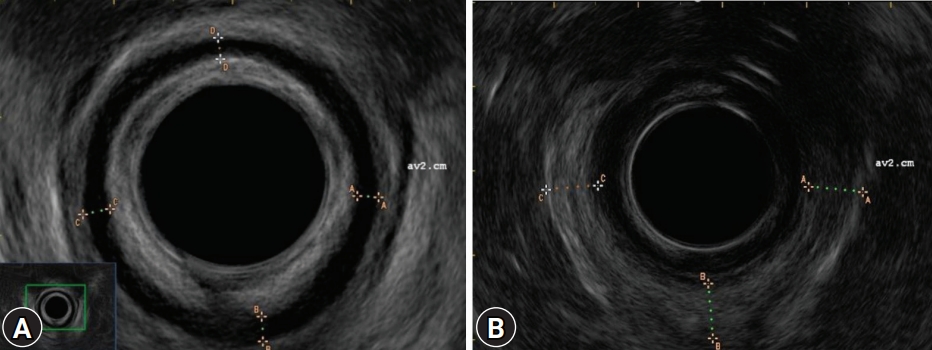
Fig. 3.Distribution plot by sex. (A) Internal anal sphincter (IAS) 2 cm from anal verge. (B) External anal sphincter (EAS) 2 cm from anal verge. (C) EAS 4 cm from anal verge.

Fig. 4.Scatter plots by body mass index (BMI). (A) Internal anal sphincter (IAS) 2 cm from anal verge. (B) External anal sphincter (EAS) 2 cm from anal verge. (C) EAS 4 cm from anal verge.

Table 1.Demographics of the study sample
|
Characteristic |
Data |
|
Age (yr) |
37 (20–77) |
|
20–30 |
7 (19.4) |
|
31–40 |
14 (38.9) |
|
41–50 |
5 (13.9) |
|
51–60 |
5 (13.9) |
|
61–70 |
4 (11.1) |
|
71–80 |
1 (2.8) |
|
Sex, male:female |
19:17 |
|
Body mass index (kg/m2) |
23.5 (17.2–31.2) |
|
Wexner score |
0 (0–2) |
Table 2.Transanal ultrasonographic findings between males and females
|
Variable |
Male |
Female |
p-value |
|
IAS thickness, 2 cm from anal verge (mm) |
1.7 (0.8–4.3) |
2.0 (1.0–3.4) |
0.622 |
|
Anterior |
2.8 (0.7–4.3) |
2.1 (1.3–3.4) |
0.131 |
|
Left lateral |
1.9 (1.2–3.2) |
1.9 (1.1–2.9) |
0.645 |
|
Posterior |
1.7 (0.8–3.8) |
1.6 (1.0–2.6) |
0.726 |
|
Right lateral |
1.9 (0.8–4.3) |
1.9 (1.2–2.8) |
0.849 |
|
EAS thickness, 2 cm from anal verge (mm) |
6.5 (5.9–8.0) |
6.4 (5.6–7.8) |
>0.999 |
|
Left lateral |
6.7 (5.9–8.4) |
6.4 (5.7–7.7) |
0.459 |
|
Posterior |
6.6 (6.0–7.7) |
6.5 (5.6–7.8) |
0.822 |
|
Right lateral |
6.8 (5.9–8.0) |
6.4 (5.8–7.6) |
0.388 |
|
EAS thickness, 4 cm from anal verge (mm) |
7.4 (6.2–8.4) |
7.2 (5.8–8.8) |
0.495 |
|
Left lateral |
7.5 (6.2–8.4) |
7.2 (5.8–8.6) |
0.469 |
|
Posterior |
7.1 (6.3–8.2) |
7.2 (5.8–8.8) |
0.822 |
|
Right lateral |
7.5 (6.4–8.4) |
7.4 (6.0–8.8) |
0.388 |
References
- 1. National Health Insurance Service (NHIS). Main surgery statistical yearbook for 2019 [Internet]. Wonju: NHIS; 2020 [cited 2021 Sep 14]. https://www.nhis.or.kr/nhis/together/wbhaec06800m01.do?mode=view&articleNo=10803657&article.offset=0&articleLimit=10.
- 2. Volløyhaug I, Taithongchai A, Arendsen L, van Gruting I, Sultan AH, Thakar R. Is endoanal, introital or transperineal ultrasound diagnosis of sphincter defects more strongly associated with anal incontinence? Int Urogynecol J 2020;31:1471–8.ArticlePubMedPMC
- 3. Walsh KA, Grivell RM. Use of endoanal ultrasound for reducing the risk of complications related to anal sphincter injury after vaginal birth. Cochrane Database Syst Rev 2015;2015:CD010826.ArticlePubMedPMC
- 4. Visscher AP, Felt-Bersma RJ. Endoanal ultrasound in perianal fistulae and abscesses. Ultrasound Q 2015;31:130–7.ArticlePubMed
- 5. Burnett SJ, Bartram CI. Endosonographic variations in the normal internal anal sphincter. Int J Colorectal Dis 1991;6:2–4.ArticlePubMed
- 6. Nielsen MB, Hauge C, Rasmussen OO, Sørensen M, Pedersen JF, Christiansen J. Anal sphincter size measured by endosonography in healthy volunteers. Effect of age, sex, and parity. Acta Radiol 1992;33:453–6.ArticlePubMed
- 7. Enck P, Heyer T, Gantke B, Schmidt WU, Schäfer R, Frieling T, et al. How reproducible are measures of the anal sphincter muscle diameter by endoanal ultrasound? Am J Gastroenterol 1997;92:293–6.PubMed
- 8. Law PJ, Bartram CI. Anal endosonography: technique and normal anatomy. Gastrointest Radiol 1989;14:349–53.ArticlePubMed
- 9. Nielsen MB, Pedersen JF, Hauge C, Rasmussen OO, Christiansen J. Endosonography of the anal sphincter: findings in healthy volunteers. AJR Am J Roentgenol 1991;157:1199–202.ArticlePubMed
- 10. Huebner M, Margulies RU, Fenner DE, Ashton-Miller JA, Bitar KN, DeLancey JO. Age effects on internal anal sphincter thickness and diameter in nulliparous females. Dis Colon Rectum 2007;50:1405–11.ArticlePubMedPMC
- 11. Frudinger A, Halligan S, Bartram CI, Price AB, Kamm MA, Winter R. Female anal sphincter: age-related differences in asymptomatic volunteers with high-frequency endoanal US. Radiology 2002;224:417–23.ArticlePubMed
Citations
Citations to this article as recorded by

- Anal Sphincter Defect and Fecal Incontinence
Sherief Mansi, Karla Vaz, Neha R. Santucci, Khalil El-Chammas, Kahleb Graham, Nelson G. Rosen, Ajay Kaul
JPGN Reports.2022; 3(4): e254. CrossRef

 , Sohyun Kim2
, Sohyun Kim2 , Sung Il Kang2
, Sung Il Kang2



 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine


 PubReader
PubReader ePub Link
ePub Link Cite
Cite





